Rhythms Originating from the Atrium
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
- Several abnormal rhythms are caused by foci conducting impulses from areas other than the sinoatrial (SA) node.
- Rhythms originating outside the sinoatrial node but within the atria are recognizable due to P wave size and shape.
- Rhythms originating from the atria are termed “supraventricular” because they originate above the ventricles.
- Atrial rhythms have a narrow QRS complex because the rhythms are supraventricular.
SA Node Irregularity
When the SA node fails to generate an impulse, a site outside the SA node but within the atria will generate an action potential faster than the SA node. The heart switches to the next fastest inherent rate beyond the SA node.
If the SA node isn’t functioning, the atrial focus initially takes over, becoming the predominant pacemaker. The atria generates impulses which travel towards the Purkinje fibers via the atrioventricular junction before heading to the ventricles the same way they would if the signal came from the SA node.
If the rate is faster than 100 beats per minute (bpm), the term “atrial tachycardia” describes the rhythm. If the rate is less than 100 bpm, it’s an “ectopic atrial” rhythm.
Impulses originating in the atrium change the normal morphology of the P wave. The atrial P wave is slower than the sinus P wave, and its morphology may be flattened, notched, or peaked. It has a saw-tooth or biphasic appearance.
A biphasic wave may produce a positive and negative deflection within one P wave. Rhythms originating from the atria will also have a narrow QRS complex because the impulses are generated above the ventricles.
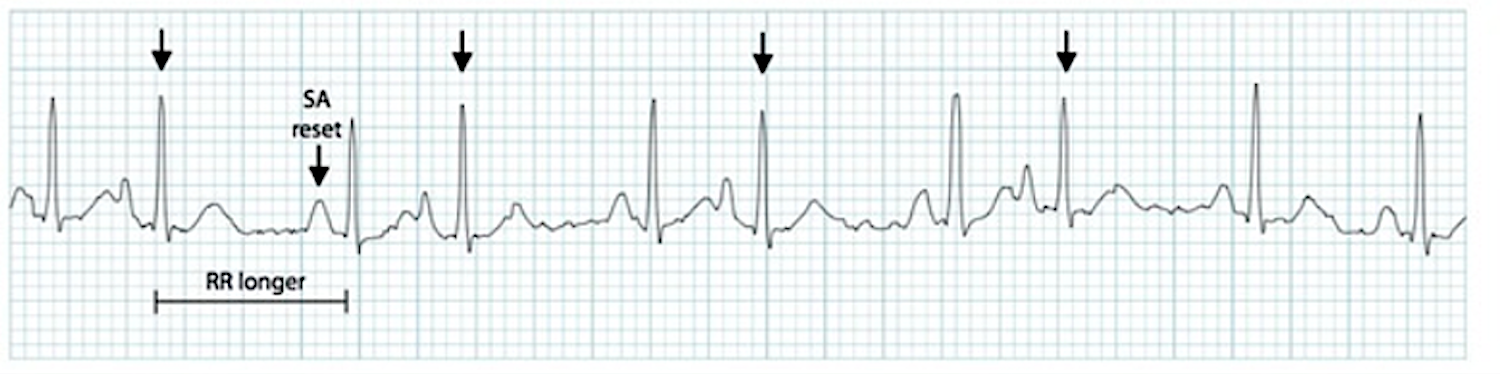
A wandering pacemaker has different foci of impulse generation throughout the atrium, switching between the sinoatrial node, atrium, and atrioventricular junction. The resulting rhythm is a combination of sinus and atrial beats. An impulse originating from the sinoatrial node presents a smooth, rounded P wave with an upward deflection. An impulse originating from the atrium presents a flattened, notched, or biphasic morphology. An impulse originating from the atrioventricular junction will result in a P wave which may look inverted or may be absent. The PR interval also varies as the impulse is generated from different foci. P wave morphology changes from one complex to the next on a wandering pacemaker’s ECG strip.Wandering Pacemaker
An ectopic beat is a single beat from a focus outside the SA node but within the conduction system.1 They’re not an arrhythmia but an irritability in the conduction system, generating an impulse strong enough to override the impulse generated from the SA node. An ectopic beat may originate as an impulse from an escape mechanism. An ectopic beat arising from the atria is known as an atrial ectopic.Ectopic Beat
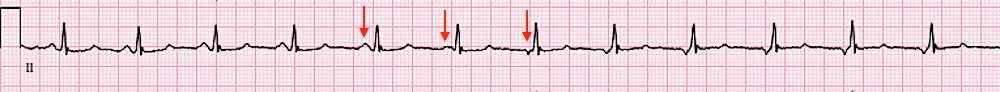
When irritability in the conduction system causes a beat to occur from an area in the atria other than the SA node, it’s a premature atrial contraction (PAC). ECG strip detailing a premature atrial contraction (PAC). PACs usually occur as a single beat. Clinicians should report the core or underlying rhythm and the type of ectopic beat (i.e., normal sinus rhythm with PAC) when reporting an ECG interpretation with a premature atrial contraction. A PAC may make the rhythm appear irregular, yet the clinician still measures R-R intervals on the 6-second strip to determine if the core rhythm is regular or irregular. The above strip details several PACs and the rhythm is quite irregular. PACs may appear in patterns, such as every other beat (bigeminy) or every third beat (trigeminy). It is also possible a PAC occurs near the end of the QRS complex and the P wave, manifesting near the T wave. It may be entirely lost within the T wave. The below strip illustrates how the T wave appears more peaked than others.Premature Atrial Contraction
Related Video – One Quick Question: What are PACs (Premature Atrial Contractions)? Video
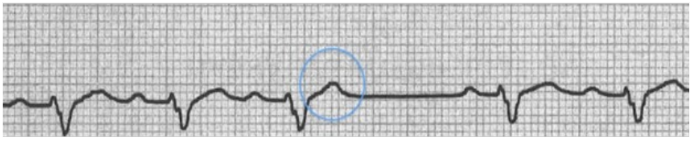
A PAC presents with a peaked T wave on an ECG.
PACs are supraventricular in nature (they occur above the ventricles), so the QRS complex must be less than 0.12 seconds.2
- RATE: depends on the core rhythm
- RHYTHM: depends on the core rhythm, which is interrupted when the PAC occurs
- P WAVE: flattened, notched, peaked or biphasic; it may occur near, or be buried within, the T wave
- PR INTERVAL: 0.12–0.20 seconds or longer
- QRS COMPLEX: less than 0.12 seconds
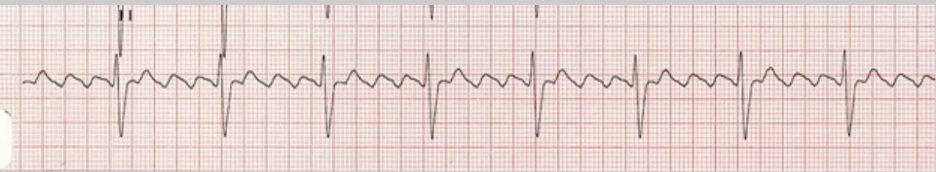
An irritable focus within the atria causes atrial tachycardia.3 The impulse generated is greater than the impulse from the SA node, the normal pacemaker of the heart. Individual complexes in atrial tachycardia have the characteristics of a PAC, including P wave morphology, PR-interval, and QRS complex. However, atrial tachycardia involves every beat instead of a single beat. Atrial flutter and multifocal atrial tachycardia are atrial tachycardia subtypes. An ECG strip illustrating multifocal atrial tachycardia (MAT) with impulses originating in multiple foci within the atria. The arrows point to P waves with unusual morphology. Atrial tachycardia is a regular arrhythmia with heart rates of 150–350 bpm.Atrial Tachycardia

Related Video – ECG Rhythm Review – Atrial Tachycardia
Read: Rhythms Originating from The Sinus Node
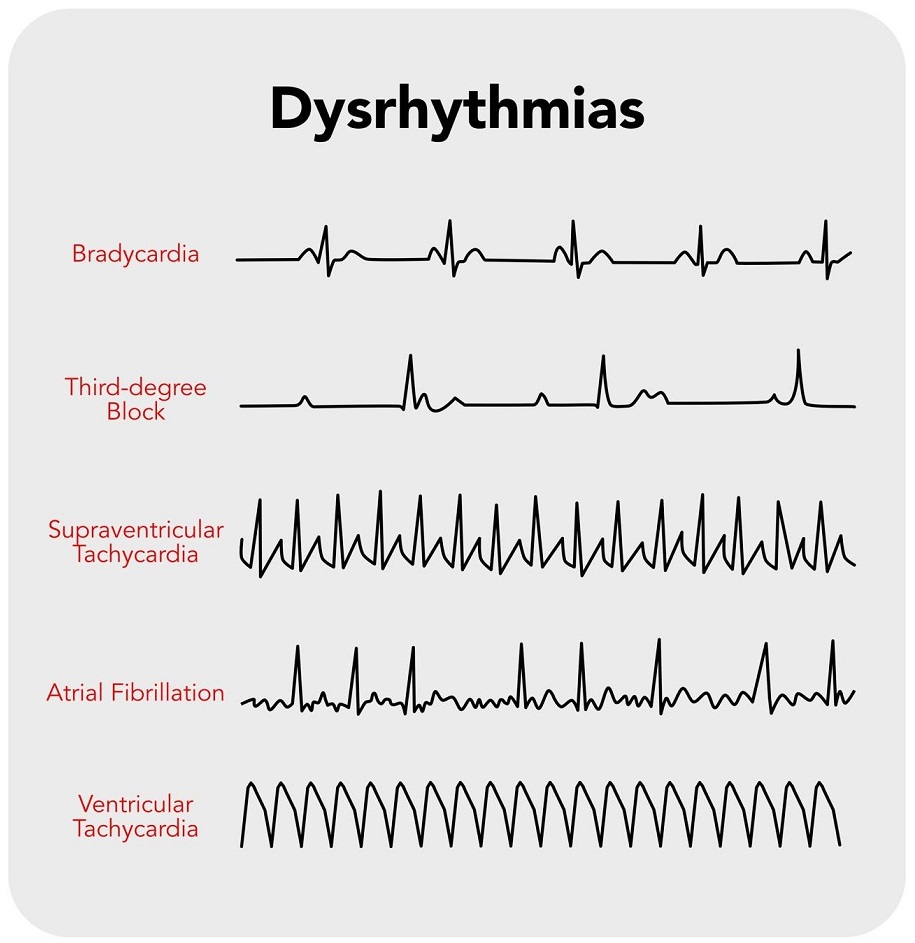
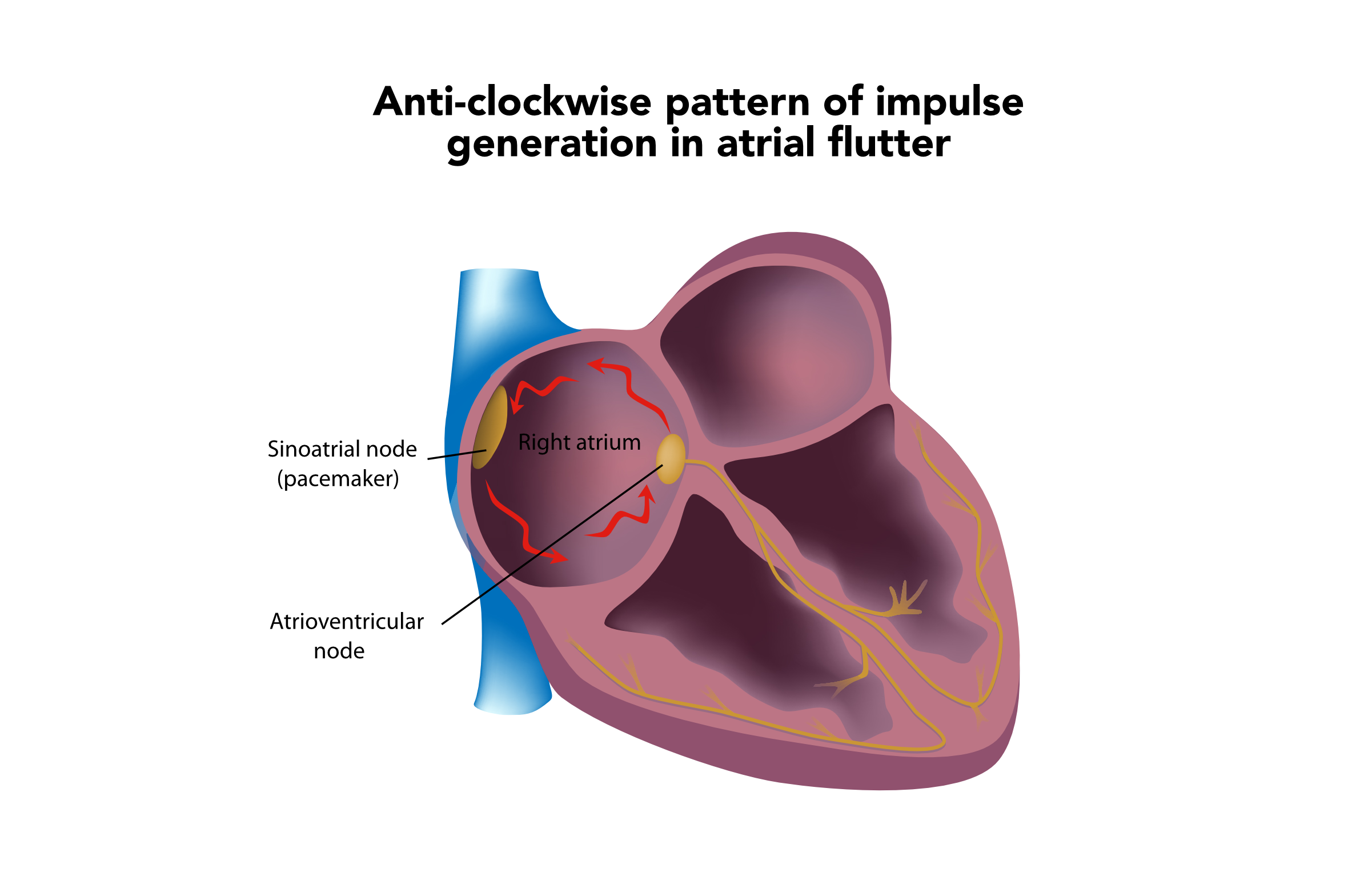
When the atria are intensely irritable, a cardiac rate above 250–350 bpm may occur. The irritability causes a rhythm known as atrial flutter, represented by a saw-tooth appearance of the P waves due to the cyclic pattern of generated impulses creating a series of rapid atrial waves. An anti-clockwise pattern of impulse generation reveals a negative deflection of the P wave on the LEAD II. If the impulse generated flows in an anti-clockwise manner, LEAD II shows a negative deflection of P waves. When the rapid rate occurs, the ventricles do not have enough time to adequately fill, so there is not enough blood volume ejected to sufficiently meet the body’s needs. Fortunately, the atrioventricular node (AV node) regulates the heart, blocking some impulses from reaching the ventricles. That allows the ventricles to fill for adequate ejection into the systemic circulation. The AV node allows impulses to pass through every second, third, or fourth P wave.4 A 12-lead ECG will detail a rapid succession of P waves with a rate between 250 and 350 bpm. A QRS complex does not follow every P wave, only manifesting every second, third, or fourth saw-tooth wave. That causes a slower ventricular rate compared to the atrial rate. The QRS complex only manifests every two, three, or four saw-tooth waves, creating a 2:1, 3:1, or 4:1 block. If the R-R interval is irregular, variable blocks are occurring.Atrial Flutter
A 3:1 block with an atrial rate of 250 bpm and a ventricular rate of 65 bpm.
In atrial flutter, the PR interval is not measured because it cannot be determined from the ECG strip. The QRS complex is normal at 0.12 seconds.
- RATE: atrial rate of 250–350 bpm; ventricular rate varies
- RHYTHM: atrial rhythm is regular; ventricular rhythm is usually regular but may be irregular if a variable block is present
- P WAVE: saw-tooth appearance
- PR INTERVAL: cannot be determined
- QRS COMPLEX: less than 0.12 seconds
Related Video – ECG Rhythm Review – Atrial Flutter
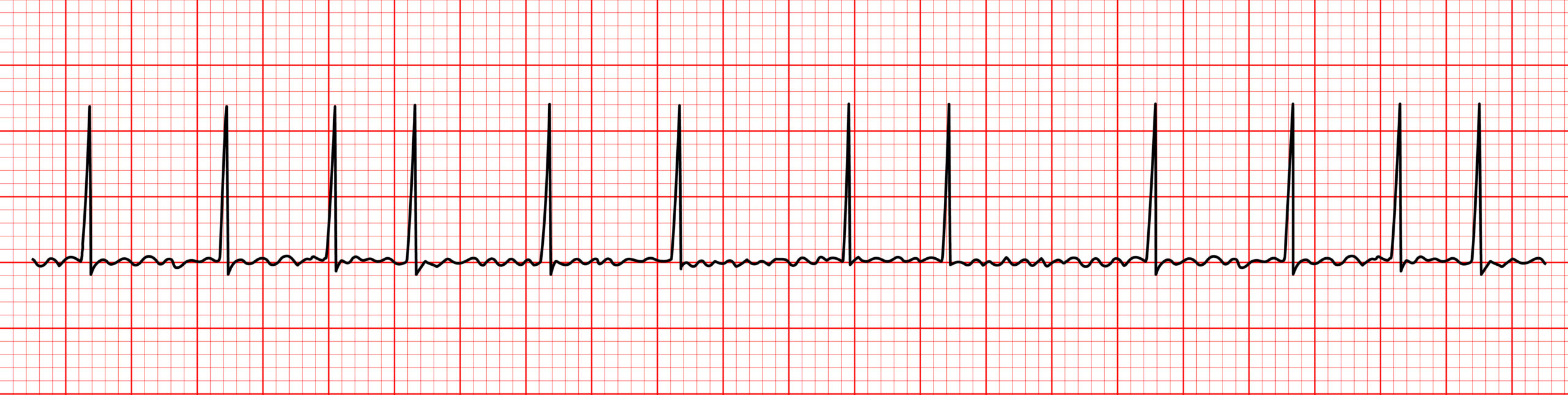
During atrial fibrillation, the atria are so intensely irritable they no longer beat but merely quiver.5 The ECG tracing displays barely visible fibrillatory waves within the isoelectric line, known as F waves. The quivering atria generate an impulse up to 350 bpm. There are no discernable P waves in atrial fibrillation. The ventricular rate is produced by the AV node blocking most of the generated impulses, producing an irregular R-R interval pattern. The F waves are generated in such a chaotic manner no discernable pattern is produced. In atrial fibrillation, the R-R interval pattern is irregular. Atrial fibrillation is easily recognized. The only two characteristic findings are the absence of P waves and irregular rhythms resulting from irregular R-R intervals. As the ventricular rate increases, R-R intervals may become closer and appear to have a regular rhythm. A rapid ventricular rate above 100 bpm (or uncontrolled ventricular response) may induce symptoms in the patient, while a ventricular rate lower than 100 bpm (or controlled ventricular response) is less likely to cause symptoms. Atrial fibrillation symptoms result from the quivering atria’s inability to fill with adequate blood, resulting in reduced cardiac output.Atrial Fibrillation
Related Video – ECG Rhythm Review – Atrial Fibrillation
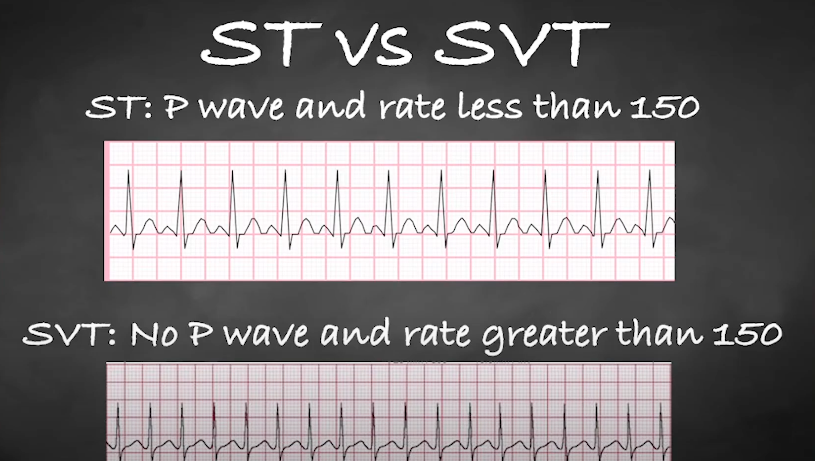
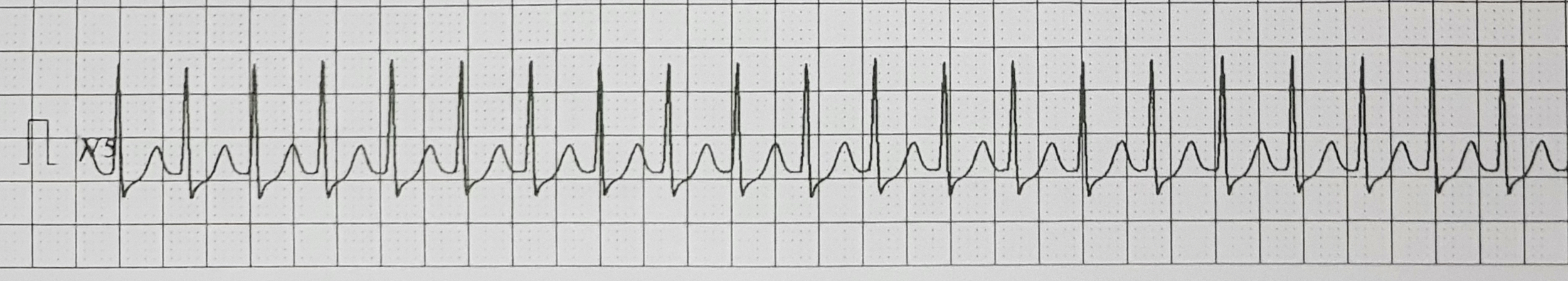
Supraventricular tachycardia (sometimes referred to as paroxysmal supraventricular tachycardia, or PSVT) is a regular tachyarrhythmia with absent P waves, arising from either the atria or AV node.6 The rate is usually 150–250 bpm. Due to the rhythm’s rapidity, patients are often symptomatic due to decreased cardiac output. The rhythm is rapid, regular, absent of P waves, and easily recognized. The QRS complex is narrow as the rhythm arises above the ventricles. Supraventricular tachycardia features absent P waves.Supraventricular Tachycardia
Related Video – One Quick Question: What are the SVT (Supraventricular Tachycardia) Criteria?
Related Video – One Quick Question: What are the Differences Between ST (sinus tachycardia) and SVT?
Related Video – ECG Rhythm Review – Supraventricular Tachycardia (SVT)
The foci sometimes conduct impulses from areas other than the SA node, creating abnormal rhythms in the atrium. These rhythms include wandering pacemakers, ectopic beats, atrial tachycardia, atrial flutter, atrial fibrillation, and paroxysmal supraventricular tachycardia. They all have different rates, rhythms, P wave ECG placement, PR intervals, and QRS complexes. Clinicians should know the different values to effectively diagnose and treat patients.Summary
More Free Resources to Keep You at Your Best
Editorial Sources
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.
1. Markham Heid. What Is an Ectopic Beat? WebMD. 2022.
2. Joseph Heaton; Srikanth Yandrapalli. Premature Atrial Contractions. National Library of Medicine. 2021.
3. Johns Hopkins Medicine. Atrial Tachycardia.
4. Joseph Heaton; Amandeep Goyal. Atrioventricular Node. National Library of Medicine. 2021.
5. Rachel Nall, MSN, CRNA. Improving Your Atrial Fibrillation Prognosis. healthline. 2021.
6. Laryssa Patti; John V. Ashurst. Supraventricular Tachycardia. National Library of Medicine. 2022.