Pharmacology Flashcard 2
Rationale
C. Rationale: If an IV or IO line cannot be established, then the last resort for drug delivery is through the ET tube.
Question
If an intravenous or intraosseous line cannot be established, the last resort for drug delivery is given:
a. Intraocular
b. Transdermal
c. Through the ET tube
d. None of the above
Answer
c. Through the ET tube
Rationale
D. Rationale: All of these are indications for the use of IV nitroglycerin in STEMI.
Question
IV nitroglycerin use in STEMI is indicated for:
A. Chest pain unresponsive to sublingual or spray nitroglycerin
B. STEMI complicated by pulmonary edema
C. STEMI complicated by hypertension
D. All of the above
Answer
D. All of the above
Rationale
A. Rationale: Vasoactive drugs impact the cardiovascular system by causing chronotropic effects (increasing heart rate), inotropic effects (myocardial contractility), vasoconstrictive effects (arterial pressure changes), or vasodilator effects (afterload reduction).
Question
What effects do positive inotropic medications have on the heart?
a. Increase myocardial contractility
b. Reduce afterload
c. Increase heart rate
d. Decrease heart rate
Answer
a. Increase myocardial contractility
Rationale
A. Rationale: Epinephrine to treat cardiac arrest is recommended to be given as a 1 mg dose of a 1:10,000 dilution IV or IO every 3 to 5 minutes. Studies have shown that this standard dose was responsible for improved survival and ROSC.
Question
What is the dosage of epinephrine given in the treatment of cardiac arrest?
a. 1 mg every 3–5 minutes
b. 2 mg every 3–5 minutes
c. 1 mg before every pulse recheck
d. A 2 mg single dose before every defibrillator shock
Answer
a. 1 mg every 3–5 minutes
Rationale
D. Rationale: The preparation of epinephrine used for CPR is a 1:10,000 dilution at a dose of 1 mg IV followed by a 10 mL NS flush. The 1:1,000 dilution is used for anaphylactic shock.
Question
What is the recommended dilution of epinephrine used for cardiopulmonary resuscitation?
a. 1:1 dilution
b. 1:10 dilution
c. 1:1,000 dilution
d. 1:10,000 dilution
Answer
d. 1:10,000 dilution
Rationale
B. Rationale: The schedule of epinephrine administration is to give 1 dose every 3 to 5 minutes, beginning 3 minutes after CPR has started.
Question
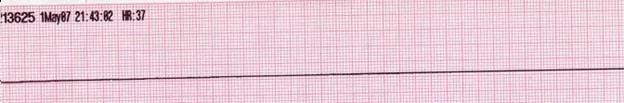
What is the timing of epinephrine administration when performing advanced cardiac life support measures in patients with cardiac arrest secondary to asystole?
a. Give one dose every 1 minute
b. Give one dose every 3 to 5 minutes
c. Give one dose after 5 cycles of CPR
d. Give one dose every 10 minutes
Answer
b. Give one dose every 3 to 5 minutes
Rationale
C. Rationale: Epinephrine can effectively increase the myocardial and cerebral blood flow during CPR through its α-adrenergic stimulating effects.
Question
What property of epinephrine makes it a drug of choice for cardiac arrest?
a. sodium channel blockade
b. anticholinergic properties
c. α-adrenergic receptor stimulating properties
d. β-adrenergic receptor blocking properties
Answer
c. α-adrenergic receptor stimulating properties
Rationale
C. Rationale: The intraosseous route is a comparable alternative to intravenous cannulation. The medullary sinusoids of long bones have direct access to the central venous circulation. The intraosseous route requires additional equipment and should be performed by experienced personnel.
Question
When intravenous cannulation is unsuccessful, which is the next best route for administering medications?
a. Subcutaneous
b. Endotracheal
c. Intraosseous
d. Intramuscular
Answer
c. Intraosseous
Rationale
C. Rationale: Amiodarone is given for shock-refractory ventricular fibrillation or pulseless ventricular tachycardia. This means that, after giving the third shock and the patient’s shockable rhythm fails to convert to normal sinus rhythm, the clinician can then give the first dose of amiodarone as a 300 mg IV bolus. Subsequently, it can be given at a lower dose of 150 mg.
Question
When is amiodarone 300 mg IV administered during ACLS resuscitation of cardiac arrest patients?
a. As a substitute for epinephrine when it is not available
b. For hypotensive post-cardiac arrest patients
c. For shock-refractory ventricular fibrillation
d. For patients with nonshockable cardiac arrest rhythms
Answer
c. For shock-refractory ventricular fibrillation
Rationale
B. Rationale: The internal jugular vein or the subclavian vein are feasible routes for central venous catheterization. The advantage of this route is that it has direct access to the central venous circulation so that the medication effects are almost instantaneous. However, this procedure is time-consuming and may prolong interruptions in the delivery of chest compressions.
Question
Which of the following anatomical structures is a viable access point for central venous catheterization?
a. Superior vena cava
b. Internal jugular vein
c. Femoral vein
d. Brachial vein
Answer
b. Internal jugular vein