Coronary Artery Disease vs. Peripheral Artery Disease
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
- Coronary artery disease (CAD) is a narrowing of the coronary arteries caused by atherosclerosis.
- The classic sign of peripheral artery disease (PAD) is intermittent claudication.
- Read on to learn about the pathophysiology, unique signs and symptoms, and nursing interventions of CAD and PAD.
This article reviews the main concepts of coronary artery disease (CAD) and peripheral artery disease (PAD). The similarities and differences will be examined, along with treatment options. CAD versus PAD
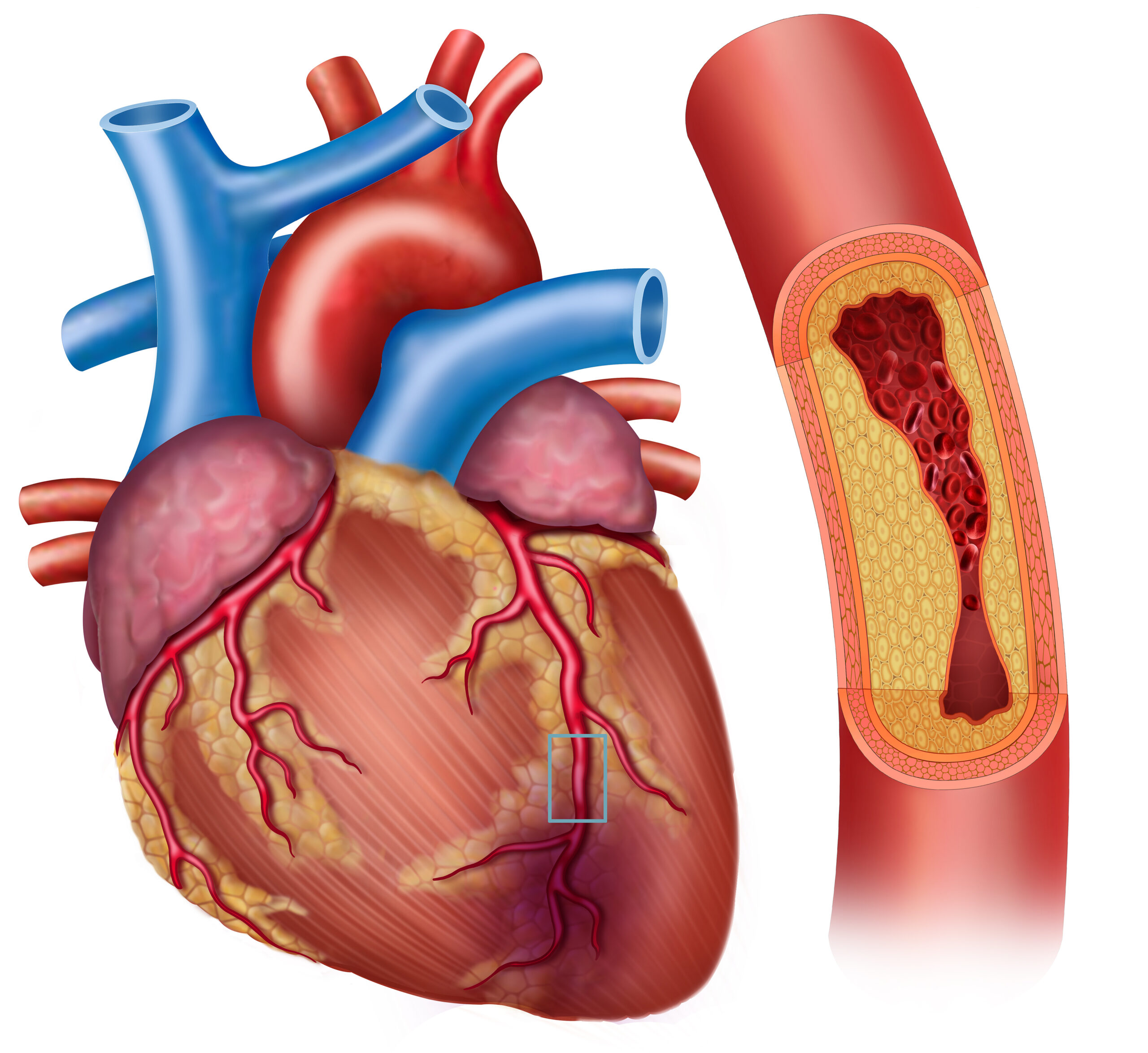
CAD is a progressive narrowing of the coronary arteries caused by atherosclerosis. To be considered CAD, the coronary arteries must be at least 70% occluded. Coronary artery disease is the build-up of plaque in the coronary arteries.What is Coronary Artery Disease?
Related Video – ACLS – Arterial Blood Gases
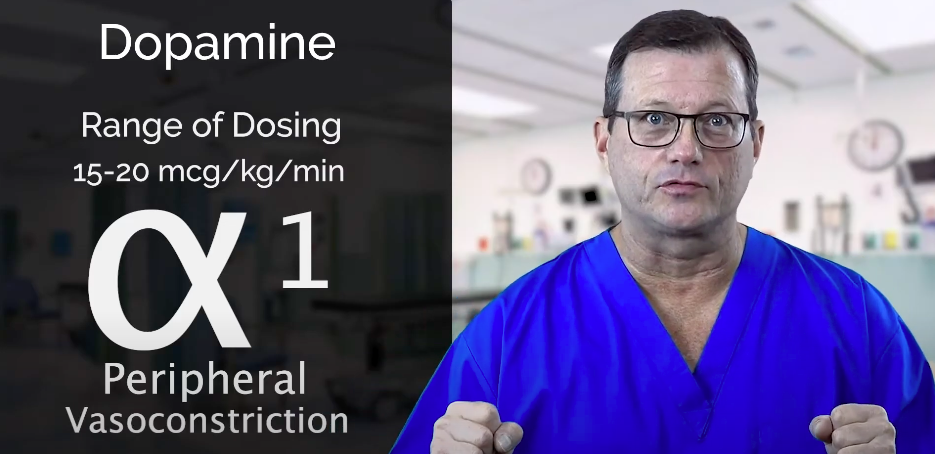
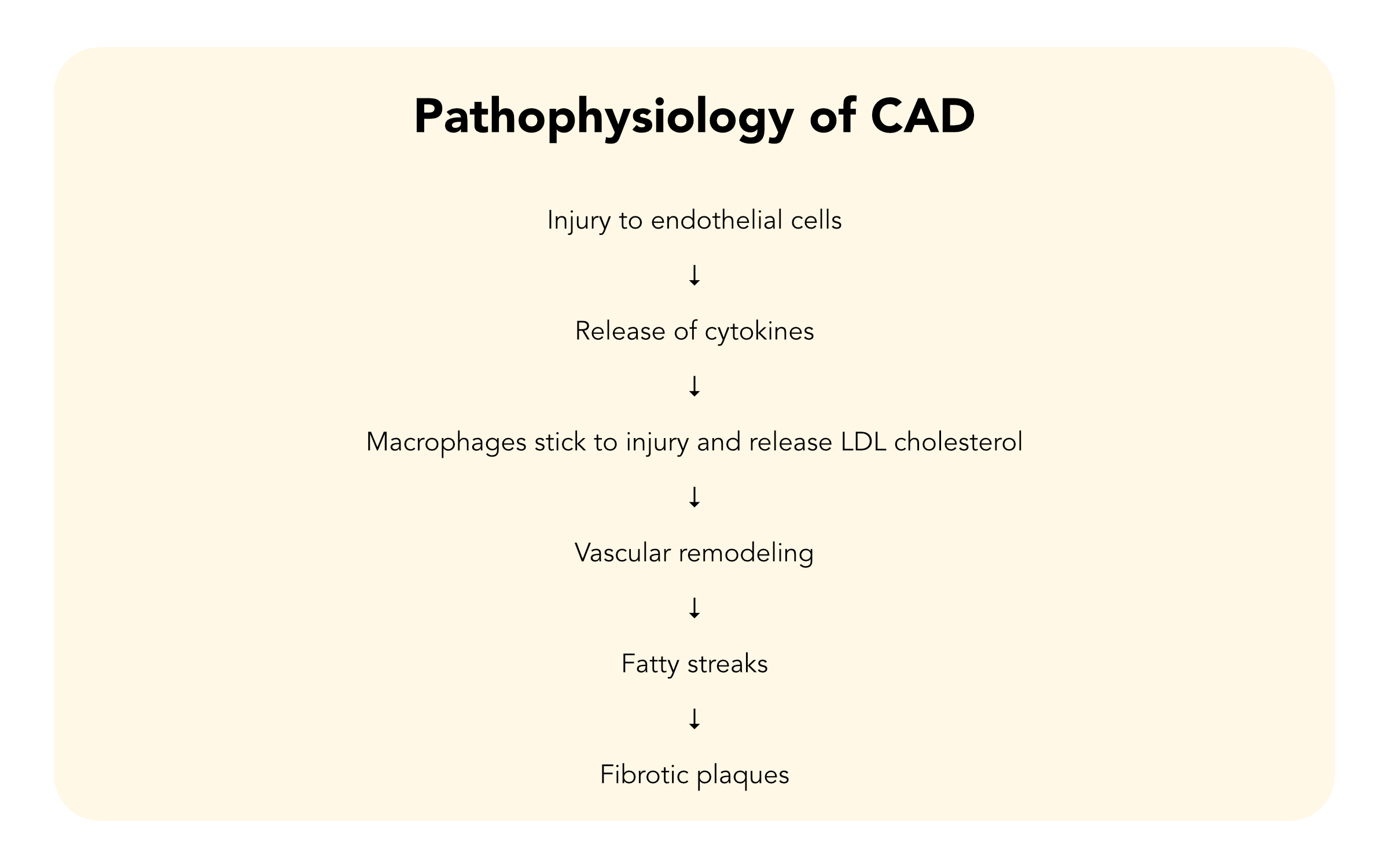
When discussing the pathophysiology of CAD, it is important to look at both the risk factors and etiologies. The risk factors of CAD include: The pathophysiology of CAD involves an inflammatory response in the lining of the coronary arteries. Any or a combination of the risk factors can set off the inflammatory response. Inflammation is intended to heal and repair when there is exposure to something that should not be there. When the inflammatory responses are set off abnormally, it is harmful to the arteries. These etiologies, or risk factors, set off the inflammatory cascade. Normally when that happens, cytokines are released. The cytokines attract macrophages to stick to that site, and they release LDL cholesterol. That LDL cholesterol is bad for the blood vessels. It is sticky, which eventually leads to the formation of fatty streaks within the inner lining of the vessels. Those fatty streaks become fibrotic plaques when “stuff” keeps building up. Eventually, the plaque ruptures and sets off the coagulation cascade, which causes the production of thrombin. When this happens, fibrinogen is converted to fibrin and platelets are attracted to the site, causing a thrombus in a coronary artery. Over time, injury to the arteries can lead to the development of plaques, or atherosclerosis. The process where plaques build up in the arteries is called atherosclerosis. Medications can help prevent the development or worsening of atherosclerosis. The most common medications are antiplatelets and aspirin. Clopidogrel (Plavix®) is an antiplatelet that prevents platelet aggregation. The concern in CAD is if the fibrotic plaque ruptures and triggers the coagulation cascade. This causes a thrombus in the coronary arteries. The thrombus can potentially lead to partial or complete occlusion of the coronary artery, causing infarction, which is known as acute coronary syndrome or myocardial infarction.Pathophysiology of CAD
The keystone of treatment for CAD is lifestyle changes, especially if it has not yet developed into a myocardial infarction. Interventions are aimed at preventative measures. Medication and procedures are also used if needed. Some of the recommended lifestyle interventions include: Medications used in the treatment of CAD include lipid-lowering agents and other cardiac drugs. Read: Hyperosmolar Hyperglycemic Syndrome: How Is It Different From DKATreatments for CAD
This class of medications should be taken with food. Importantly, bile acid resins interfere with the absorption of other drugs. Patients need to be educated to take bile acid resins one hour before or four hours after taking other drugs.
Peripheral arterial disease (PAD) is a circulatory problem caused by narrowed arteries in the extremities, particularly the legs. The extremities do not receive enough blood flow to keep up with the demand due to the narrowed arteries.What is Peripheral Arterial Disease?
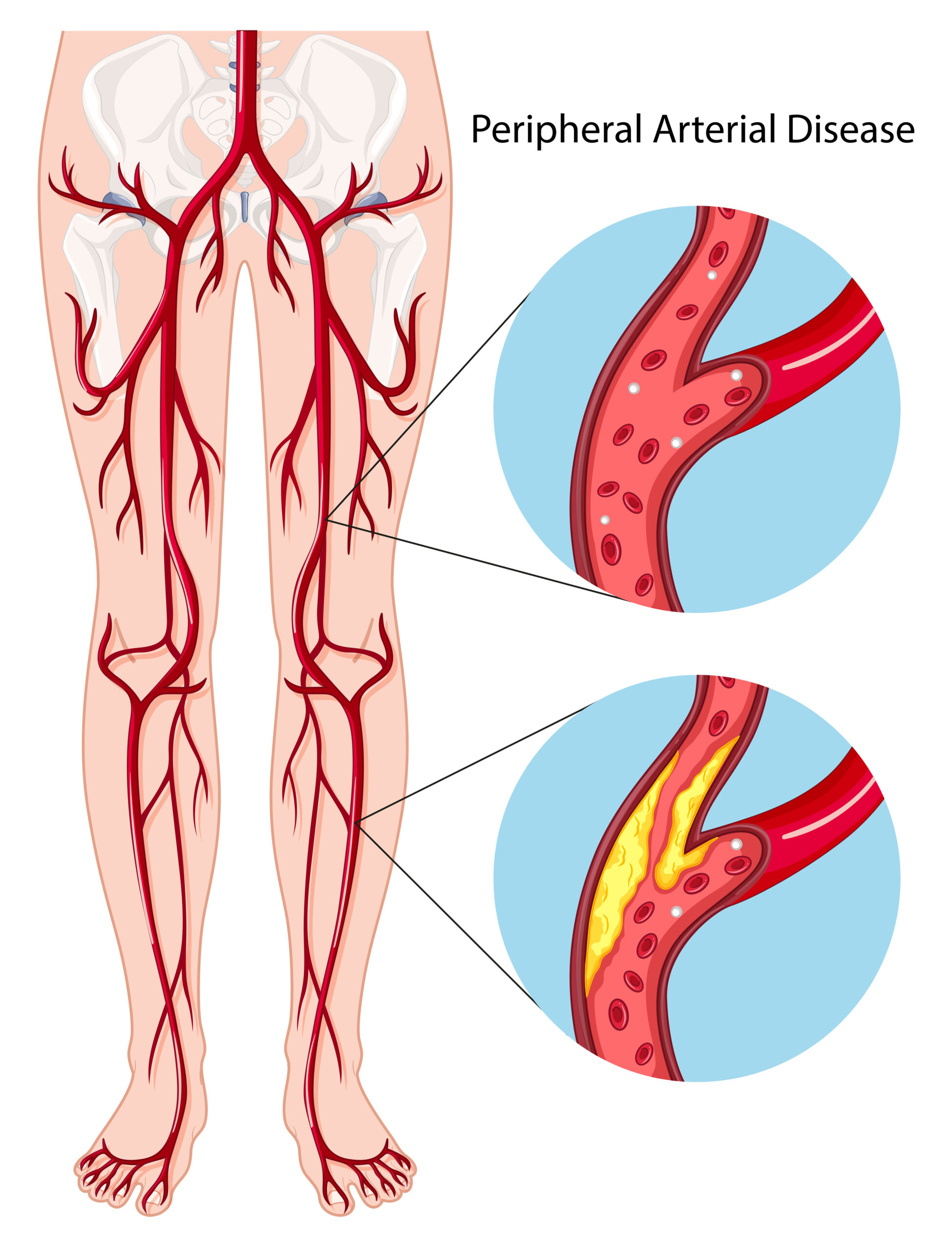
The pathophysiology of PAD is the same process as CAD. Both conditions are caused by atherosclerosis, the process that leads to narrowing of the arteries. The difference between PAD and CAD is which blood vessels are affected. In CAD, the coronary arteries are affected. In PAD, the arteries that feed the lower legs and feet are impacted. There are two classifications of PAD: When a patient’s foot does not have adequate blood flow for a long period, the foot will not be healthy. It will lack hair, the skin will look flaky, and the toenails will dry and scale off. Peripheral arterial disease is caused by atherosclerosis in the peripheral arteries.Pathophysiology of PAD
Related Video – One Quick Question: How Do You Calculate Mean Arterial Blood Pressure?
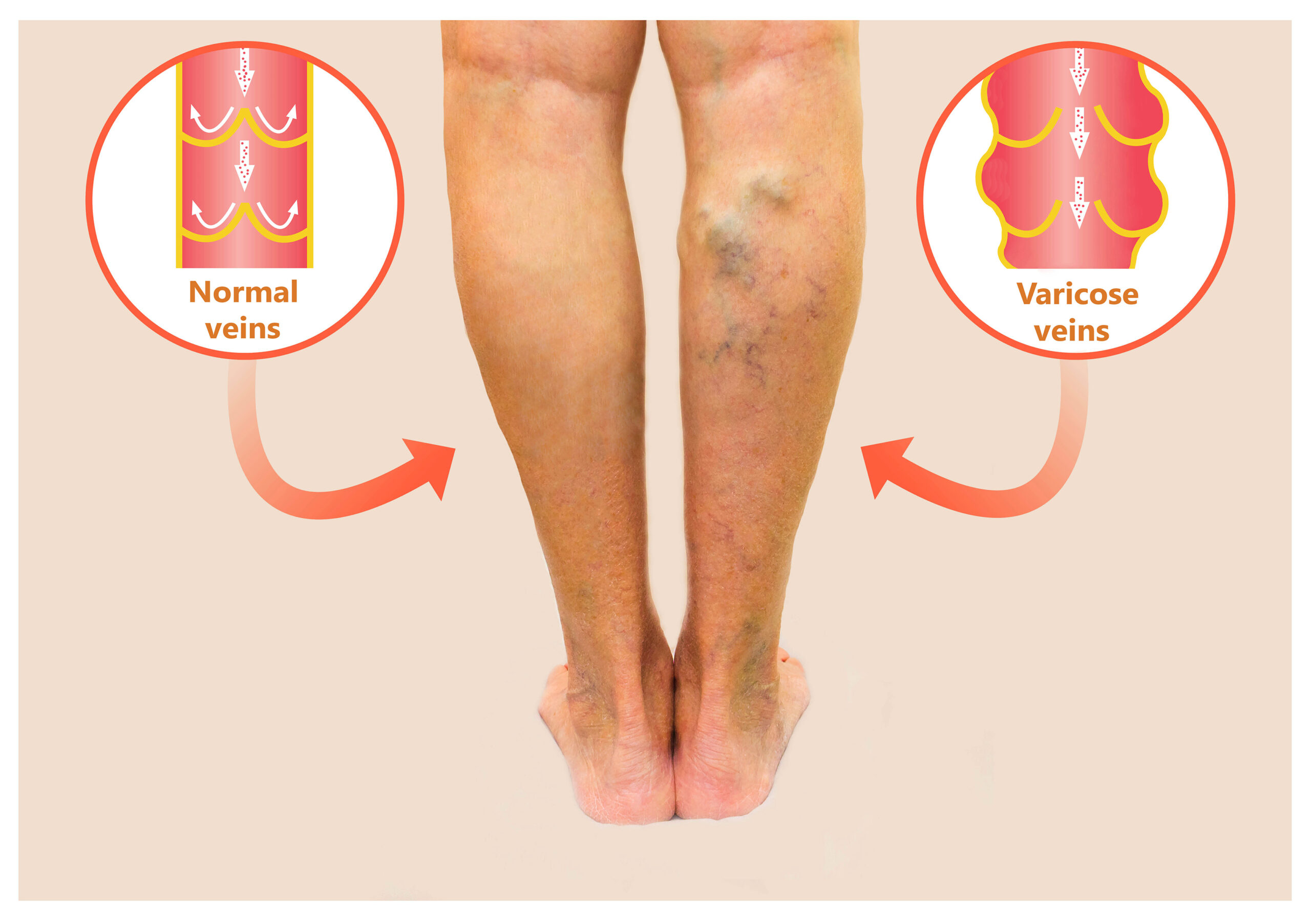
What is the difference between PAD and peripheral venous insufficiency? PAD is a blood flow issue, while peripheral venous insufficiency is a blood return issue. In PAD, the body does not have adequate blood flow to the extremities. The classic signs and symptoms are paresthesia, neuropathic pain, and tingling. The skin is cool to the touch and pallor. There is low hair growth. Another sign is pulselessness. It is usually difficult to find the pedal pulse and may require use of a Doppler. If a patient has an ulcer, the ulcer will have a “punched out” appearance with clean and clear borders, usually presents on the outside of the ankle without swelling. Ulcers are common on the outside of the foot in peripheral arterial disease. With peripheral venous insufficiency, blood is getting to the limbs but not returning properly. The most common cause of venous insufficiency is varicose veins. Another cause is incompetent valves. Signs and symptoms of peripheral venous insufficiency include edema, pain that improves when the legs are raised, a “messy” ulcer, and swelling. The ulcer may be brown in color with drainage. The ulcer will typically be located at the medial malleolus or the inside of the ankle. Varicose veins are the most common cause of peripheral venous insufficiency.Clarifying the Difference between PAD and Peripheral Venous Insufficiency
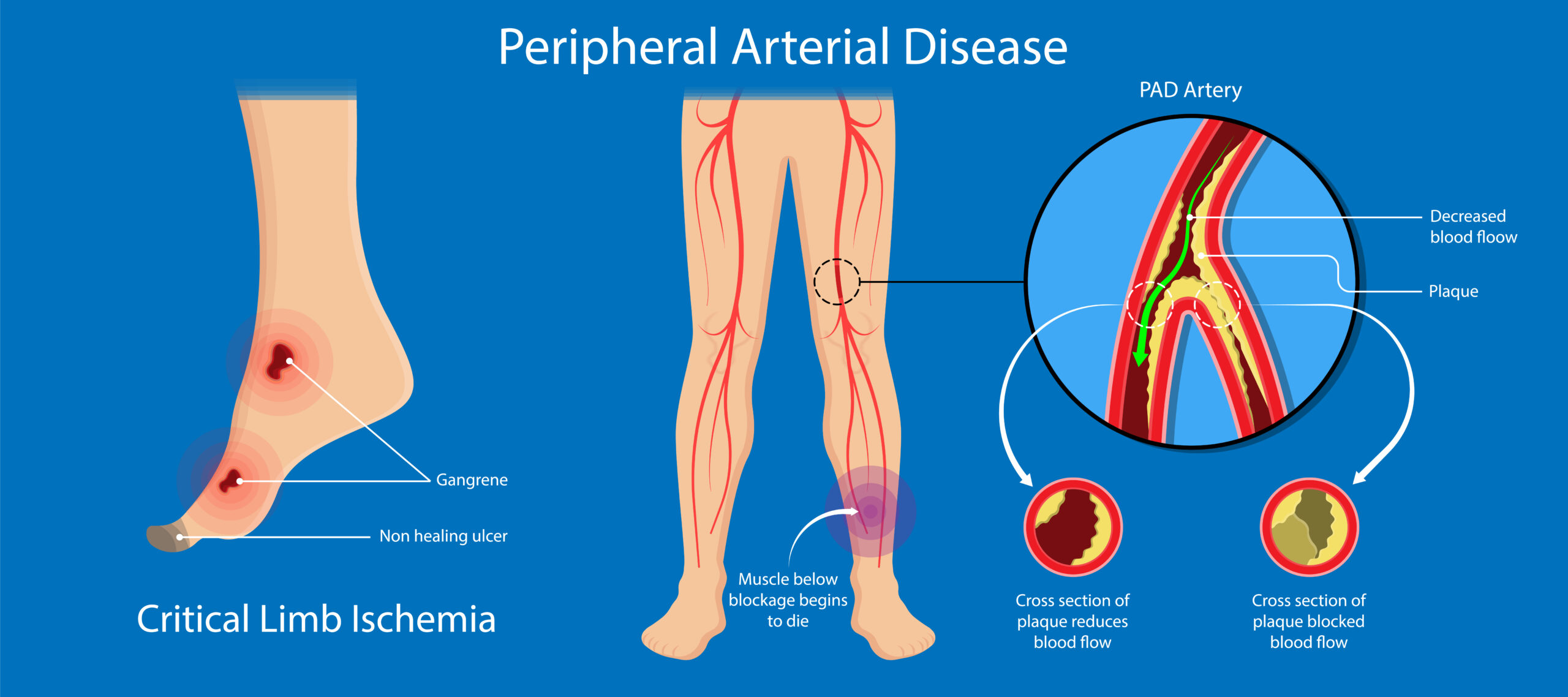
Since PAD is a blood flow issue, the nursing care involves:Nursing Care for PAD
Treatment for PAD consists of lifestyle interventions, medications, and potentially surgery. Lifestyle interventions for PAD are similar to those for CAD. Lifestyle interventions that help manage and reduce the progression of PAD are: Some medications used in the treatment of PAD include: Pentoxifylline and cilostazol help to reduce the pain of intermittent claudication. They are used for symptom management but do not cure PAD. CAD is a progressive narrowing of the coronary arteries caused by atherosclerosis. PAD is a circulatory problem caused by narrowed arteries in the extremities, particularly the legs. Both conditions result in decreased blood flow, and it is important to understand the pathophysiology of these diseases and the ways they are treated to provide guidance and treatment.Treatments for PAD
More Free Resources to Keep You at Your Best
Editorial Note
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.