Basics of Ventilators: Part 1
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
- Ventilators are machines that help a patient breathe.
- Important terminology to know when working with ventilators is minute ventilation, tidal volume, and respiratory rate.
- Read on to learn about the basics of ventilators.
This article provides a basic introduction to ventilators. Ventilators are life support machines that help a patient inhale and exhale. Sometimes they are called “breathing machines.” Ventilators are commonly used in the intensive care unit (ICU). Patients will be placed on ventilators if they have respiratory or neurological conditions that make them unable to breathe on their own. This article introduces ventilators and includes: Ventilators are machines that help a patient inhale and exhale.Ventilator Settings

Related Video – What is Adaptive Support Ventilation?
Before reviewing ventilator settings, it is important to introduce the terminology to understand respiratory physiology and the way ventilators are designed to help patients breathe. The following terms will be defined below: Minute ventilation (MV) is the volume of air a patient breathes every minute, with normal values ranging from 5–8 liters per minute. Minute ventilation is the product of tidal volume (TV) and respiratory rate (RR): MV = TV × RR Tidal volume is the volume of air someone takes in with each breath. Normal tidal volumes range from 6–8 mL/kg and range between 500 to 700 mL. Respiratory rate is the number of breaths a person takes per minute. A normal RR for an adult is 12–16 breaths per minute. For example, in a patient who weighs 70 kg with a tidal volume of 480 mL with each breath and a respiratory rate of 14 breaths per minute, the total volume of air the patient takes in per minute would be 6,720 mL (6.72 L). Tidal volume and respiratory rate can be adjusted on a ventilator to achieve a specified minute ventilation for the patient. Lung compliance is defined as the lung’s ability to expand and stretch. It is calculated by the change in volume divided by the change in pressure: Lung compliance = ∆Volume/∆Pressure The patient’s lung compliance dictates the ability of the ventilator machine to deliver the specified volume of air. Often, patients in the ICU will present with pathologies that alter lung compliance, such as: The patient’s lung compliance dictates the ability of the ventilator machine to deliver the specified volume of air. Often, patients in the ICU will present with pathologies that alter lung compliance, such as: I:E ratio stands for inspiratory to expiratory ratio. Normally, the I:E ratio is 1:2, which means that inspiration is about half as long as expiration. The I:E ratio should be adjusted depending on the disease process. For example, in a patient with emphysema, the expiratory time may be lengthened, so the patient receives an I:E ratio of 1:3. In a patient with ARDS, the inspiratory time should be increased to facilitate the contact time between the alveolar bed and the capillary. This patient would receive an I:E ratio of 2:1. Plateau pressure is the pressure applied to the airway in the absence of airflow and a good indicator of a patient’s lung compliance. Peak pressure reflects the resistance to airflow and is measured during inspiration when the ventilator is delivering air to the patient. When both peak and plateau pressures are high, it is a sign that a patient’s lung compliance is poor. If peak pressures are high while plateau pressures are normal, this indicates there is an airway obstruction, such as a kinked breathing tube or a mucus plug. The ventilator delivers the necessary volume of air based on the patient’s lung compliance. Read: Basics of Ventilators: Part 2Understanding the Terminology

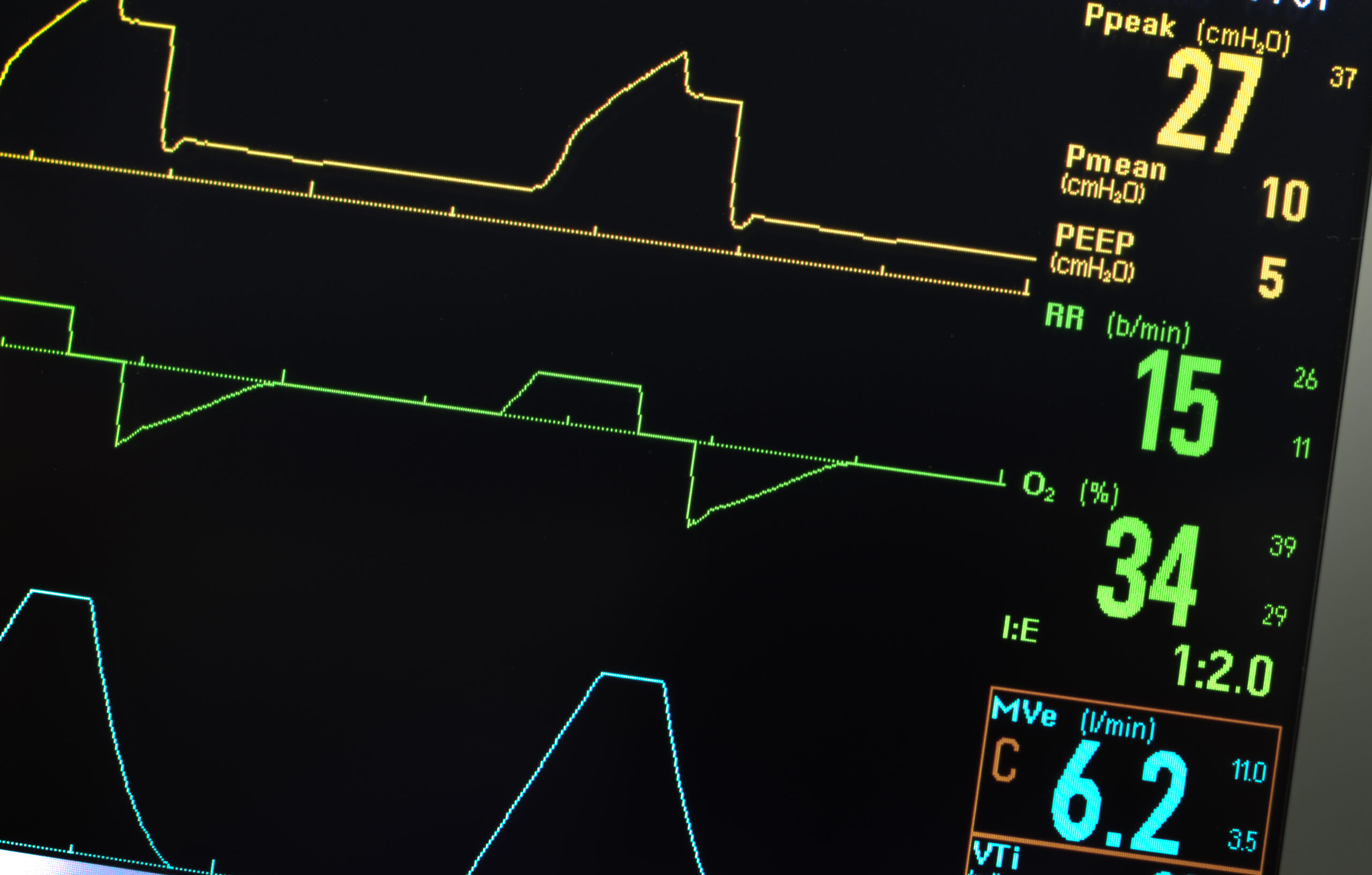
To comprehend ventilator settings, the provider must understand why a ventilator machine is used. Ventilators assist the patient in achieving oxygenation and ventilation. The term oxygenation describes the role of delivering oxygen to the patient. The term ventilation is used to describe removing carbon dioxide from the patient. To control oxygenation, the ventilator has two adjustable variables: A patient breathing room air takes in a FiO2 of 21%. On the ventilator, the FiO2 can be set up to 100%, but the goal should always be to aim for a lower FiO2, setting based on the patient’s tolerance. PEEP is the pressure the machine applies to the patient’s lung at the end of expiration. The pressure prevents the alveoli from completely collapsing, which allows them to stay open to take in air (inspiration) and provide more oxygen to the patient. For example, picture a balloon that represents a single alveolus. When the balloon is filled with air (inhalation), it will attempt to expel air as it is stretched to its limit. That represents the start of expiration. When the balloon shrinks and lets out air (exhalation), the balloon collapses. PEEP is the pressure applied to prevent the balloon from completely shrinking and collapsing. To control ventilation, the tidal volume and respiratory rate can be adjusted. By maintaining a normal minute ventilation (MV = TV RR), the ventilator can dictate how much carbon dioxide the patient exhales. A ventilator monitor displays several aspects of the patient’s breathing. Note the PEEP, I:E ratio, and minute ventilation (MVe).Two Mechanical Ventilator Settings
Related Video – Tips for Bagging
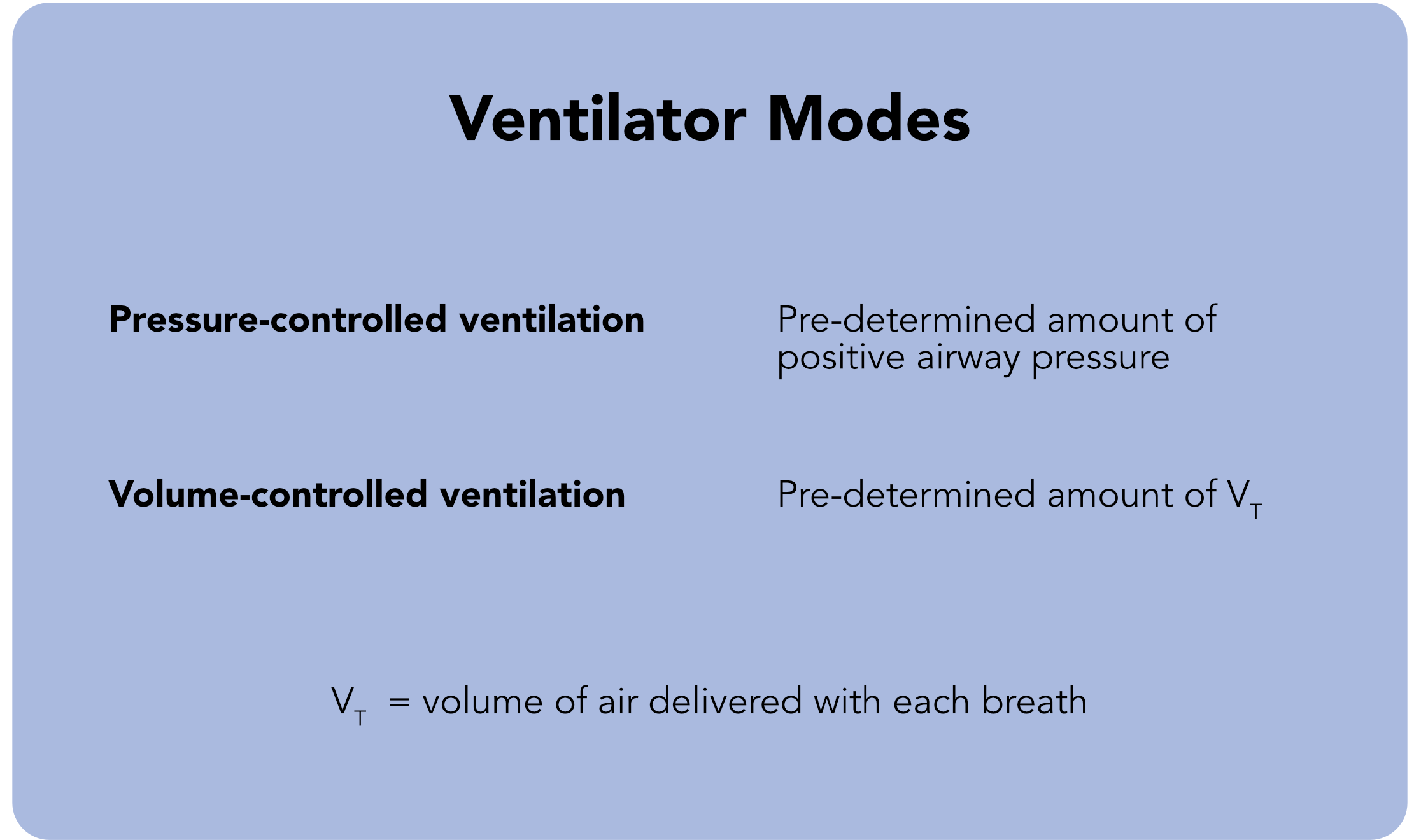
The volume of air delivered to the patient, or the tidal volume, can be delivered through two broad ventilatory modes: Ventilator Modes In pressure-controlled ventilation, the inspiratory pressure of air is adjusted to achieve the specified tidal volume. For example, if the peak inspiratory pressure is at 20 mm Hg and a tidal volume of 400 mL, the peak inspiratory pressure can be adjusted up or down to achieve the desired tidal volume. The advantages of pressure-controlled ventilation are that oxygenation is favored by controlling peak inspiratory pressures, and the risk of barotrauma (barotrauma risk > 30 mm Hg) is decreased. The major disadvantage is that there are no guarantees that the target volume of air can be achieved no matter how high the pressure is increased. Volume-controlled ventilation is the opposite of pressure-controlled ventilation. In this mode, the desired tidal volume is preset, and the ventilator will achieve this volume by exerting a set pressure. For example, if the goal is to deliver a tidal volume of 450 mL to a patient, then the machine will adjust and deliver this volume at a peak pressure of 22 mm Hg. The advantage of this mode is that the ventilator will deliver a guaranteed volume to the patient. However, the disadvantage is that it favors ventilation over oxygenation. As the tidal volume increases, the expiratory time to breathe that volume out also increases. What this means for the patient is that the expiratory time is greater than inspiratory time. This article has introduced basic information about ventilators, including important terminology, ventilator settings, and the two types of ventilation for mechanical ventilators. Be sure to check out Ventilators Part 2 for further discussion on the various ventilator modes.Ventilator Modes
Related Video – Ventilator Basics – Part 2
More Free Resources to Keep You at Your Best
Editorial Note
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.