AV Rhythms Flashcard 1
Rationale
A. Rationale: Atrioventricular blocks delay conduction or completely block impulses from the atria to the ventricles. They are brought about by an increase in vagal tone, which is elicited during sleep, athletic training, pain, or stimulation of the carotid sinus. Vomiting and dizziness are not known to elicit AV blocks. Severe hypokalemia may trigger ventricular arrhythmias.
Question
Which of the following is a potential cause of an AV block?
a. Carotid sinus stimulation
b. Vomiting
c. Dizziness
d. Hypokalemia
Answer
a. Carotid sinus stimulation
Rationale
A. Rationale: AVNRT is paroxysmal, meaning it occurs suddenly and spontaneously resolves. In the common form of AVNRT, the slow pathway traverses the antegrade direction, while the fast pathway traverses the retrograde direction. This causes the atria (the receiving end of the retrograde impulse) and the ventricles (the receiving end of the antegrade impulse) to be activated at approximately the same time.
Question
A patient with atrioventricular nodal reentrant tachycardia has slow impulses traversing the antegrade direction, while the second fast pathway traverses the retrograde direction. What is the net effect of this electrophysiological change?
a. The atria and ventricles are activated at the same time.
b. The atria will be activated much faster than the ventricle.
c. The ventricles will be activated much faster than the atria.
d. Neither the atria nor the ventricles will be activated.
Answer
a. The atria and ventricles are activated at the same time.
Rationale
C. Rationale: A junctional rhythm that exceeds the rate of 100 bpm is known as junctional tachycardia. A junctional rhythm with a rate of 60–100 bpm is known as an accelerated junctional rhythm. A junctional escape rhythm has an inherent rate of 40–60 bpm.
Question
An irritable AV junctional rhythm can be disrupted and override the SA node or higher pacemaker site that will cause an increase in the rate of depolarization. Which of the following is a junctional rhythm with a rate that exceeds 100 bpm?
a. Junctional escape rhythm
b. Premature junctional complex
c. Junctional tachycardia
d. Accelerated junctional rhythm
Answer
c. Junctional tachycardia
Rationale
A. Rationale: AVNRT can be influenced by premature atrial beats with first-degree atrioventricular block. AVNRT has two pathways that can be used as a re-entry circuit. One is conducted in an antegrade direction, while the other is conducted in a retrograde direction. Each pathway may have a slow component or a fast component.
Answer choice B – A premature ventricular beat is an early contraction caused by an irritated electrical focus within the ventricles, not the atria.
Answer choice C – A right bundle branch block manifests as a prolonged QRS complex due to a delay in electrical conduction within the right bundle branch.
Answer choice D – A left bundle branch block manifests as a prolonged QRS complex due to a delay in electrical conduction within the left bundle branch.
Question
Atrioventricular nodal re-entrant tachycardia (AVNRT) is produced via two pathways, a slow component pathway and a fast component pathway within the atrioventricular node. Which one of the following can elicit AVNRT?
a. Premature atrial beat
b. Premature ventricular beat
c. Right bundle-branch block
d. Left bundle-branch block
Answer
a. Premature atrial beat
Rationale
B. Rationale: The AV node anatomy has a “dual pathway” in patients with AVNRT. A reentry circuit confined to the AV node and the atrial tissue around it has caused a regular supraventricular tachycardia. The QRS complex in AVNRT is narrow (< 0.12 seconds), indicating normal ventricular activation via the His-Purkinje system. This is the common AVNRT variant. Sometimes aberrant conduction occurs, which can result in a wide QRS complex. This aberrant conduction can be a bundle branch block.
Question
How many atrioventricular nodal pathways does a patient with atrioventricular nodal reentrant tachycardia have?
a. 1
b. 2
c. 3
d. 4
Answer
b. 2
Rationale
A. Rationale: Once the sinoatrial node fails to produce an impulse, the heart switches to the next fastest inherent rate. An atrial focus has the next fastest inherent rate, followed by the AV node, then the bundle of His, and lastly, the bundle branches and Purkinje fibers.
Question
If the sinoatrial node fails to form an impulse, where should the next predicted impulse originate?
a. Atria
b. Bundle of His
c. Purkinje fibers
d. Right bundle branch
Answer
a. Atria
Rationale
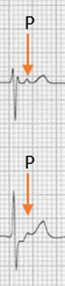
C. Rationale: In atypical AVNRT, the fast conduction is directed in the antegrade direction, while the slow component travels in the retrograde direction. The activation of the atria will occur last. There will be negative P waves in the inferior leads III and aVF. This is seen late, after the QRS complex. The “RP interval” is longer than the PR interval.
Answer choice A – Second-degree AV block, Mobitz Type I will appear as a PR interval that prolongs before a QRS complex is dropped after a non-conducted P wave.
Answer choice B – Second-degree A block, Mobitz Type II will appear as a constant PR interval with regularly non conducted P waves.
Answer choice D – In typical AVNRT, the fast conduction is directed in the retrograde direction, while the slow component travels in the antegrade direction.
Question
Refer to the image below. An ECG configuration with a QRS-P-T complex is the hallmark of which one of the following arrhythmias?
a. Second-degree AV block, Mobitz type I
b. Second-degree AV block, Mobitz type II
c. Atypical fast-slow AVNRT
d. Typical slow-fast AVNRT
Answer
c. Atypical fast-slow AVNRT
Rationale
A. Rationale: The normal QRS duration is 0.09 seconds or less, which is equivalent to 2 small squares on an ECG. A QRS > 0.12 seconds is considered prolonged. Prolonged QRS duration has an unusual QRS pattern, such as a bundle branch block. The impulse may originate from the ventricles with atrioventricular dissociation. If the ventricular rate is low, it is known as a ventricular escape rhythm.
Answer choice B – Idioventricular rhythm is characterized by a heart rate < 50 bpm, the absence of P waves, and a wide QRS complex.
Answer choice C – An idioventricular rhythm exhibits a slow heart rate.
Answer choice D – A ventricular escape rhythm exhibits a slow heart rate.
Question
Which of the following ECG characteristics is representative of atrioventricular dissociation with a slow heart rate?
a. A slow ventricular rate exhibiting a ventricular escape rhythm
b. A slow ventricular rate exhibiting an idioventricular rhythm
c. A fast ventricular rate exhibiting an idioventricular rhythm
d. A fast ventricular rate exhibiting a ventricular escape rhythm
Answer
a. A slow ventricular rate exhibiting a ventricular escape rhythm
Rationale
B. Rationale: 40% of AV blocks are brought about by ischemic heart disease. Other causes include congenital heart disease, cardiomyopathies, myocarditis, and familial diseases.
Question
Which of the following is the most common cause of AV blocks?
a. Genetic factors
b. Ischemic heart disease
c. Cardiomyopathies
d. Myocarditis
Answer
b. Ischemic heart disease
Rationale
D. Rationale: Vagal maneuvers, intravenous adenosine, and intravenous calcium channel blockers or beta-blockers are treatment options for AVNRT. When necessary, during periods of hemodynamic instability, synchronized electrical cardioversion almost always terminates AVNRT in conjunction with the other treatments mentioned above. If there are occasions where sinus rhythm is not achieved after the initial shock, it may be necessary to perform subsequent electrical cardioversion.
Question
Which of the following is the recommended treatment for symptomatic atrioventricular nodal reentrant tachycardia?
a. Adenosine
b. Calcium channel blockers
c. Vagal maneuvers
d. All of the above
Answer
d. All of the above