Arrhythmias Flashcard 8
Rationale
C. Rationale: Bradyarrhythmia’s unlikely to respond to atropine are second-degree AV block, Mobitz type 2 and third-degree AV block with wide QRS complex that represent the block to be non-nodal.
Question
What bradyarrhythmia is unlikely to respond to atropine?
a. Second-degree AV block, Mobitz type 1
b. Third-degree AV block with a narrow QRS complex
c. Third-degree AV block with a wide QRS complex
d. None of the above
Answer
c. Third-degree AV block with a wide QRS complex
Rationale
C. Rationale: The initial dose of adenosine to be given in this case is 6 mg rapid IV push followed by a normal saline flush. A rapid IV push is necessary because of the short half-life of adenosine. A subsequent dose can be given at 12 mg.
Question
What initial dose of adenosine should be administered to a patient with a symptomatic narrow, regular QRS complex tachyarrhythmia?
a. 0.5 mg
b. 1 mg
c. 6 mg
d. 12 mg
Answer
c. 6 mg
Rationale
C. Rationale: Tachycardia is a heart rate > 100 bpm.
Question
What is the definition of tachycardia?
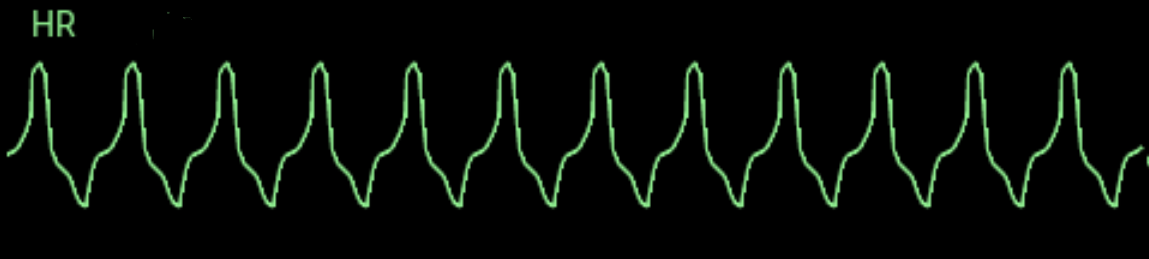
a. A heart rate < 50 bpm
b. A heart rate of 60 to 100 bpm
c. A heart rate > 100 bpm
d. A heart rate between 50 and 60 bpm
Answer
c. A heart rate > 100 bpm
Rationale
D. Rationale: Bradycardia is defined as a heart rate < 60 bpm. Patients with bradyarrhythmia will typically have symptoms when the heart rate is < 50 bpm.
Question
What is the heart rate under which patients with bradyarrhythmia will be symptomatic?
a. 40 bpm
b. 50 bpm
c. 150 bpm
d. 220 bpm
Answer
d. 220 bpm
Rationale
C. Rationale: Atropine is given via intravenous bolus administration at a dose of 1 mg. It may be repeated every 3–5 minutes if the desired effect is not reached. Do not exceed a total dose of 3 mg.
Question
What is the maximum total dose of atropine in the treatment of symptomatic bradyarrhythmia’s?
a. 1 mg
b. 2 mg
c. 3 mg
d. 4 mg
Answer
c. 3 mg
Rationale
D. Rationale: Atropine is an anticholinergic drug. It blocks acetylcholine, thereby inhibiting the parasympathetic nerve impulses and allowing the heart rate to increase. To be specific, atropine is also an antimuscarinic drug because it antagonizes the muscarine-like actions of acetylcholine.
Question
What is the mode of action of atropine in the treatment of symptomatic bradycardia?
a. Beta-2 agonist
b. Potassium-channel blocker
c. Fast sodium-channel blocker
d. Anticholinergic
Answer
d. Anticholinergic
Rationale
D. Rationale: Atropine improves the heart rate and the signs and symptoms associated with bradycardia.
Question
What is the pharmacologic therapy of choice for a patient with a myocardial infarction that has caused ischemia in the sinoatrial node and has induced symptomatic bradycardia?
a. Amiodarone
b. Aspirin
c. Albuterol
d. Atropine
Answer
d. Atropine
Rationale
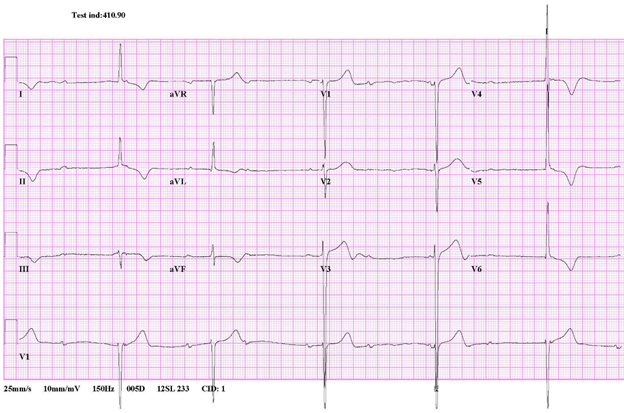
B. Rationale: If a shock is delivered in a tachyarrhythmia during the refractory period of the cardiac cycle, ventricular fibrillation can be produced. Synchronized cardioversion avoids this effect by delivering the shock during the peak of the QRS complex.
Question
What treatment for tachyarrhythmias aims to restore the normal heart rhythm with a pulse by delivering its effect that is timed at the peak of the QRS complex?
a. Defibrillation
b. Synchronized cardioversion
c. Precordial thump
d. Rapid IV administration with adenosine
Answer
b. Synchronized cardioversion
Rationale
B. Rationale: If the patient does not have a pulse, you should immediately proceed to the ACLS Cardiac Arrest algorithm.
Question
When treating a patient with tachycardia, the first step is:
a. Evaluate rhythm
b. Check pulse
c. IV, O2, and monitor
d. Evaluate blood pressure
Answer
b. Check pulse
Rationale
C. Rationale: Atropine is given at a dose of 1.0 mg IV every 3 to 5 minutes until a total dose of 3 mg has been administered. (ACLS Case: Symptomatic Bradycardia)
Question
When treating symptomatic bradycardia, atropine is given at a dose of 1.0 mg IV every 3 to 5 minutes to a maximum dose of:
a. 1 mg
b. 2 mg
c. 3 mg
d. 4 mg
Answer
c. 3 mg