Arrhythmias Flashcard 5
Rationale
D. Rationale: Hyperkalemia is indicated by tall, peaked T waves, small P waves, and widened QRS complexes on an ECG. Hyperkalemia can be treated using sodium bicarbonate, calcium chloride, and/or glucose plus insulin.
Question
Effective intervention for hyperkalemia might include:
A. Sodium bicarbonate
B. Calcium chloride
C. Glucose plus insulin
D. All of the above
Answer
D. All of the above
Rationale
C. Rationale: Endpoints for the administration of procainamide include suppression of the arrhythmia, hypotension, maximum dosage reached (17 mg/kg), or widening of the QRS by 50%.
Question
Endpoints for the administration of procainamide include:
A. Duration of QRS increases by 25%
B. Maximum dose of 27 mg/kg is reached
C. Hypotension
D. Increase in heart rate by 30 points
Answer
C. Hypotension
Rationale
C. Rationale: The provider must know when to use synchronized cardioversion based on the patient’s rhythm.
Question
For which of the following unstable tachyarrhythmias is synchronized cardioversion NOT recommended?
a. Atrial flutter
b. Atrial fibrillation
c. Ventricular fibrillation
d. Supraventricular tachycardia
Answer
c. Ventricular fibrillation
Rationale
B. Rationale: The correct dose of atropine in bradycardia is 1 mg given every 3–5 minutes to a maximum dose of 3 mg. Atropine should be used cautiously in the presence of cardiac ischemia or MI as it may worsen ischemia and increase infarct size. Doses < 0.5 mg may result in a paradoxical slowing of the heart.
Question
Identify the correct dosing regimen for atropine for the treatment of symptomatic bradycardia:
A. Atropine 0.5 mg IV every 2 minutes to a maximum of 2 mg
B. Atropine 1 mg IV every 3–5 minutes to a maximum of 3 mg
C. Atropine 0.5 mg IV every 3–5 minutes to a maximum of 3 mg
D. Atropine 1 mg IV every 5 minutes; there is no maximum dosage for atropine
Answer
B. Atropine 1 mg IV every 3–5 minutes to a maximum of 3 mg
Rationale
B. Rationale: The correct order is: 1) Place pacing electrodes on the chest; 2) turn the pacer ON; 3) set the demand rate to 60 beats/min (this rate can be adjusted up or down based on the patient’s clinical response); 4) set the current milliamperes output 2 mA above the dose at which consistent capture is observed.
Question
Identify the correct sequence of steps to perform transcutaneous pacing:
A. 1) Turn the pacer ON; 2) place pacing electrodes on the chest; 3) set the demand rate to 50 beats/min; 4) set the current milliamperes output 2 mA above the dose at which consistent capture is observed.
B. 1) Place pacing electrodes on the chest; 2) turn the pacer ON; 3) set the demand rate to 60 beats/min; 4) set the current milliamperes output 2 mA above the dose at which consistent capture is observed.
C. 1) Place pacing electrodes on the chest; 2) turn the pacer ON; 3) set the demand rate to 50 beats/min; 4) set the current milliamperes output 2 mA above the dose at which consistent capture is observed.
D. 1)Turn the pacer ON; 2) set the current milliamperes output 2 mA above the dose at which consistent capture is observed; 3) set the demand rate to 60 beats/min; 4) place pacing electrodes on the chest.
Answer
B. 1) Place pacing electrodes on the chest; 2) turn the pacer ON; 3) set the demand rate to 60 beats/min; 4) set the current milliamperes output 2 mA above the dose at which consistent capture is observed.
Rationale
D. Rationale: All of these statements are correct. In some conditions, the heart compensates for decreased cardiac output by increasing the heart rate. Reducing the heart rate in these patients may lead to a worsening of their clinical condition.
Question
Identify the CORRECT statement regarding sinus tachycardia:
A. Treatment of sinus tachycardia focuses on correcting the underlying problem.
B. Sinus tachycardia is caused by external factors, such as fever, hypotension, or anemia.
C. Sinus tachycardia usually has a gradual onset and termination.
D. All of these
Answer
D. All of these
Rationale
D. Rationale: This type of tachycardia should be treated as a wide complex tachycardia until proven otherwise. This is because wide complex tachycardias are more dangerous and likely to degenerate into a terminal rhythm, e.g., ventricular fibrillation.
Question
Identify the following rhythm:
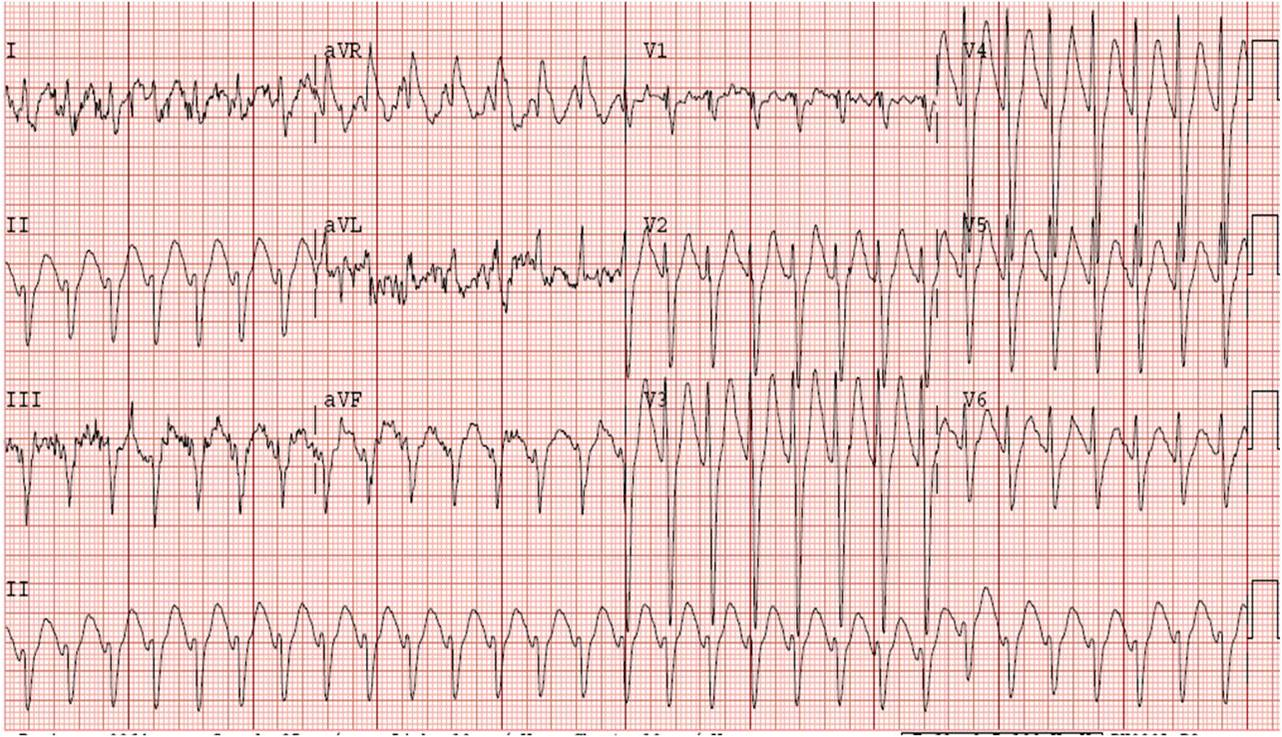
a. Ventricular tachycardia
b. Junctional tachycardia
c. Supraventricular tachycardia
d. Wide complex tachycardia of uncertain type
Answer
d. Wide complex tachycardia of uncertain type
Rationale
C. Rationale: Sodium bicarbonate is used to counter metabolic acidosis. Metabolic acidosis and hyperkalemia are two of the few indications for sodium bicarbonate use. Improving oxygenation by ventilating the patient can also help to reverse metabolic acidosis.
Question
In a patient with severe metabolic acidosis, treatment might include:
A. Intubation and optimization of ventilatory status
B. Sodium bicarbonate
C. Both of these
D. None of these
Answer
C. Both of these
Rationale
C. Rationale: Atropine is given at a dose of 1 mg IV every 3–5 minutes until a maximum total dose of 3 mg has been administered.
Question
In bradycardia, atropine is given at a dose of 1 mg IV every 3–5 minutes to a maximum total dose of how many milligrams?
a. 1 mg
b. 2 mg
c. 3 mg
d. 4 mg
Answer
c. 3 mg
Rationale
A. Rationale: Atropine is not indicated in bradycardia if the AV block is at the His-Purkinje level or in any non-nodal bradycardia. Second-degree AV block, Mobitz type I has a conduction defect at the AV node where atropine is effective. Torsades de pointes is not a bradyarrhythmia.
Question
In severe and symptomatic bradycardia, in which one of the following conditions is atropine most effective?
a. Second-degree AV block, Mobitz type I
b. Second-degree AV block, Mobitz type II
c. Torsades de pointes
d. Third-degree AV block
Answer
a. Second-degree AV