Anti-Anxiety Medications
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
- Some common anti-anxiety medications include benzodiazepines, buspirone, hydroxyzine, duloxetine, escitalopram, and propranolol.
- Different anti-anxiety medications work for different types of anxiety.
- Clinicians will learn about five common classes of medications used to treat anxiety.
Introduction to Anti-Anxiety Medications
Many types of drugs treat anxiety.
Benzodiazepines
Of all the anxiety medications, benzodiazepines are the only one prescribed exclusively for anxiety. The rest treat other illnesses such as depression or insomnia. Benzodiazepines end in “-pam,” such as clonazepam and lorazepam. They calm patients down.
Benzodiazepines directly enhance the effects of gamma aminobutyric acid (GABA), a neurotransmitter that protects the brain from overstimulation. Enhancing GABA produces drowsiness, sedation, and lethargy.
Benzodiazepines are also an effective treatment for acute anxiety attacks. They have a profound effect, and providers administer them to people with severe anxiety and panic disorders.
The most damaging potential side effect is respiratory depression. Physicians should also monitor the patient’s dependence and tolerance when they’re regularly taking benzodiazepines.
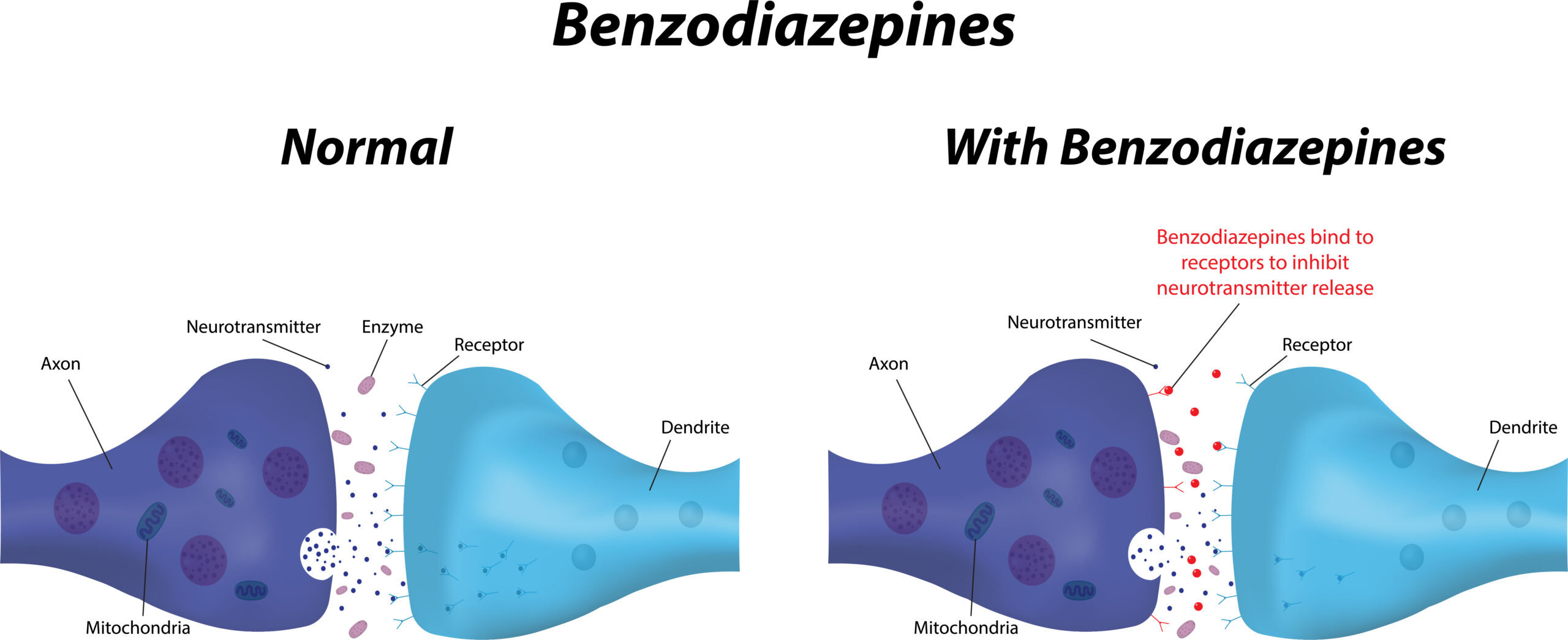
Benzodiazepines enhance the effects of GABA.
Related Video – Antidepressant Medications
Atypical Anxiolytics
The main atypical anxiolytic is buspirone (BuSpar®). It’s often prescribed for depression because it increases free levels of serotonin and dopamine, neurotransmitters thought to be low in patients who experience major depressive disorder. Those neurotransmitters have a calming effect, which helps treat the anxiety.
Buspirone will not work for acute anxiety, severe anxiety, acute panic, or severe panic. It is prescribed for generalized anxiety to control the disorder. It’s important that providers inform patients of buspirone’s potential gastrointestinal (GI) side effects. Nausea and constipation may occur, so providers should administer it with food.
Read: Dosage Calculation Explained
Antihistamines
While antihistamines include Benadryl®, there is another called hydroxyzine (Vistaril®). Providers frequently prescribe this medication for anxiety and occasionally for insomnia. The antihistamines directly block histamine receptors, causing sedation and decreasing anxiety.
Antihistamines are not used for acute panic. They’re administered for mild anxiety or performance anxiety, such as social anxiety.
Providers should inform patients of antihistamines’ possible GI side effects, especially anticholinergic side effects which dehydrate a patient. The patient may experience dry eyes, dry mouth, constipation, and abdominal cramps.
Headache is also a common side effect of hydroxyzine and other antihistamines.
Serotonin Norepinephrine Receptor Inhibitors (SNRIs) and Selective Serotonin Receptor Inhibitors (SSRIs)
Both SNRIs and the SSRIs are prescribed for depression. SNRIs increase serotonin and norepinephrine levels, while SSRIs only increase serotonin levels.
The prototype SNRI prescribed for anxiety is duloxetine and is also prescribed for neuropathic pain. The standard SSRI is escitalopram. Both duloxetine and escitalopram are also prescribed for depression.
Importantly, these drugs are not used for acute anxiety or severe anxiety. They’re administered mostly for generalized anxiety disorders.
Providers must let patients know of the similar GI side effects, especially diarrhea. Patients should take these drugs with food to minimize the side effects.
Related Video – Introduction to ACLS Medications
Non-selective Beta-blockers
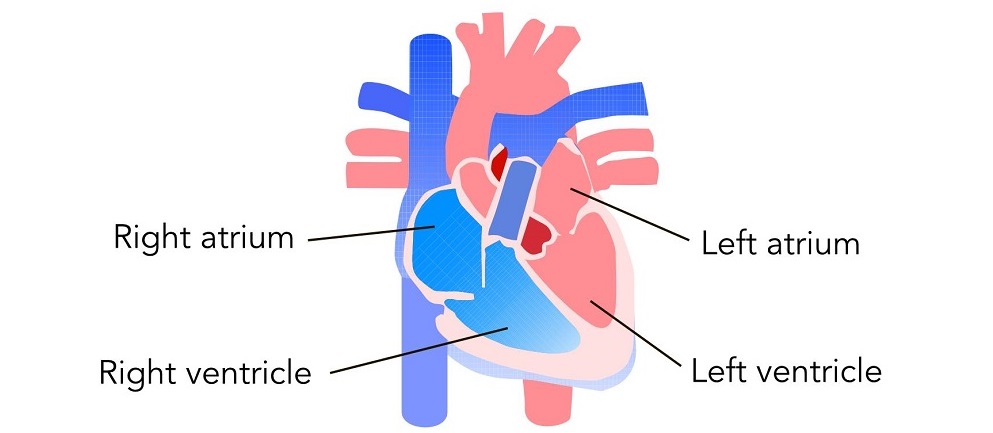
Beta-blockers block the stimulation of epinephrine and norepinephrine, calming the heart rate, dilating blood vessels, and reducing the overall heart workload.
Non-selective indicates the beta-blocker doesn’t differentiate between beta-receptors on the heart versus the lungs. Normally, when beta-receptors on the lung are activated, bronchodilation is present. However, when beta-receptors are blocked by beta-blockers, bronchoconstriction occurs.
Non-selective beta-blockers put patients at higher risk for bronchoconstriction, and they’re contraindicated in patients with respiratory disease. Providers should not administer non-selective beta-blockers to patients with asthma or severe COPD. It can send the patient into bronchoconstriction respiratory distress.
Non-selective beta-blockers are great for performance anxiety, social anxiety, and calming the symptoms associated with anxiety, as well as slowing the heart rate. They’ll also prevent the tremors and sweating associated with performance anxiety.
Propranolol is the prototype non-selective beta-blocker prescribed for anxiety. Providers must monitor the patient for hypotension, bradycardia, dizziness, and lightheadedness, especially if the patient isn’t initially hypertensive. If a patient with normal blood pressure is administered a beta-blocker, their blood pressure must be monitored.
These are the most common drug classes administered to treat anxiety disorders. The image below is an excellent summary.
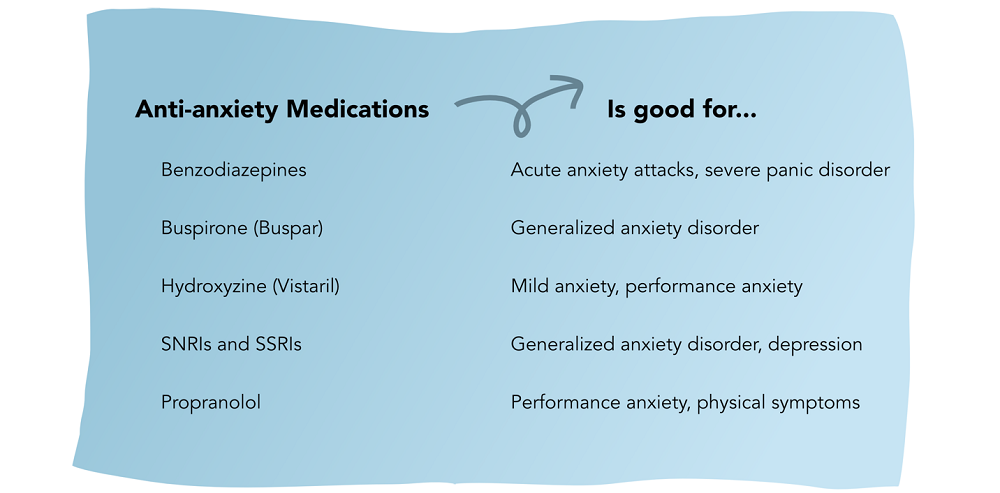
Summary of Anti-Anxiety Medications
More Free Resources to Keep You at Your Best
Editorial Note
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.