ACLS Principles Flashcard 15
Rationale
D. Rationale: All of the reversible causes of cardiac arrest can cause pulseless electrical activity. Recall the Hs and Ts mnemonic: hypoxia, hypo/hyperkalemia, hydrogen ion, hypovolemia, hypothermia, tamponade, tension pneumothorax, thrombosis (pulmonary and cardiac), and toxins. If resuscitative efforts fail to achieve a return of spontaneous circulation early, then the responders should look for possible reversible causes of cardiac arrest and immediately perform the necessary interventions.
Question
Which one of the following medical conditions can cause pulseless electrical activity?
a. Hypoxia
b. Pulmonary embolism
c. Cardiac tamponade
d. All of the above
Answer
d. All of the above
Rationale
D. Rationale: The Early Warning Score uses the following physiological parameters and assigns points for them: respiratory rate, oxygen saturation, supplementary oxygen, temperature, systolic BP, heart rate, and level of consciousness.
Question
Which one of the following physiologic parameters is used in the Early Warning Score?
a. Temperature
b. Heart rate
c. Oxygen saturation
d. All of the above
Answer
d. All of the above
Rationale
C. Rationale: Advanced directives are legal documents that may contain a do not attempt to resuscitate (DNAR) clause. It must be shown to the healthcare provider before cardiopulmonary resuscitation is commenced. Choice D is incorrect because the situation is hearsay without documentation, and CPR must be continued.
Question
Which one of the following situations includes a patient that no longer needs advanced or basic life support?
a. A person who is pulseless after drowning
b. A person hit by lightning right in front of you who is occasionally gasping
c. A geriatric patient with a confirmed advanced directive found with asystole in the ICU
d. A patient with abnormal breathing who has overdosed with opioids, and his friend tells you that he no longer wishes to be revived
Answer
c. A geriatric patient with a confirmed advanced directive found with asystole in the ICU
Rationale
C. Rationale: Studies have shown no difference in outcomes if either a shock was delivered or chest compressions were performed first.
Question
Which one of the following statements is true?
a. Outcomes are better if a shock was delivered before chest compressions.
b. Outcomes are better if chest compressions were started before a shock was delivered.
c. There is no difference in outcomes if either a shock or chest compressions were delivered first.
d. None of the above
Answer
c. There is no difference in outcomes if either a shock or chest compressions were delivered first.
Rationale
B. Rationale: A rhythm check is most appropriate to perform after 2 minutes of high-quality CPR.
Question
While resuscitating a patient in cardiac arrest with pulseless ventricular tachycardia, when do you perform a rhythm check?
a. Immediately after defibrillation
b. After 2 minutes of high-quality CPR
c. After administration of epinephrine every 3 to 5 minutes
d. Monitoring the ECG tracing for an organized rhythm is not an integral part of the cardiac arrest algorithm.
Answer
b. After 2 minutes of high-quality CPR
Rationale
B. Rationale: At this time, you must recognize that the person is in cardiac arrest. The first step is to ensure that the scene is safe. Then call for help and activate the emergency response system. An AED should be requested. Once all of these are done, the next most appropriate action is to initiate high-quality CPR.
Question
While waiting at the barbershop, an older man who recently reported having chest pain has become unresponsive with occasional gasping. You check for a pulse and feel none. What are the most appropriate steps to take at this time?
a. Monitor the patient until help arrives.
b. Call for help and activate the emergency response team; have an AED ready.
c. Perform a precordial thump.
d. Initiate high-quality CPR and use the AED when available.
Answer
b. Call for help and activate the emergency response team; have an AED ready.
Rationale
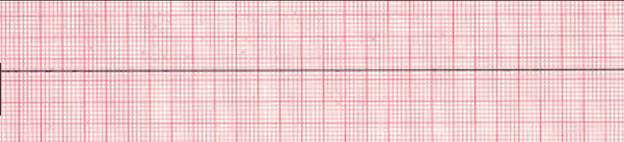
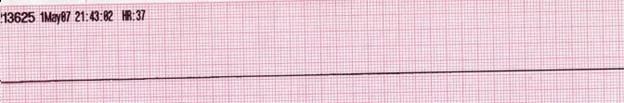
D. Rationale: When in doubt between fine ventricular fibrillation and asystole, give one shock. Fine ventricular fibrillation is a sign of prolonged arrest.
Question
You are an EMS provider and arrive at the scene of an unconscious patient with no pulse and not breathing. Your partner immediately initiates high-quality CPR while you attach the defibrillator to the patient and record the ECG. After checking that the leads are in place and the device is functioning properly, you are trying to determine if the ECG tracing is a fine ventricular fibrillation or asystole. What is your next course of action?
a. Place an advanced airway
b. Continue high-quality CPR for 2 minutes
c. Obtain intravenous access
d. Defibrillate the patient
Answer
d. Defibrillate the patient
Rationale
B. Rationale: In some situations, it may be appropriate to consider extending resuscitative efforts beyond the scope of your department’s policies. The patient’s friend is not a legal decision-maker to suggest a do not resuscitate directive. The remaining choices are situations where out-of-hospital resuscitative efforts can be terminated.
Question
You are an EMS provider and have been resuscitating a patient in cardiac arrest with asystole for more than 25 minutes. You are considering that CPR may be futile due to the prolonged resuscitative efforts that have not improved the patient’s status. Which of the following situations prompts you to continue the resuscitation until your team gets to the nearest hospital?
a. An authorization for termination of resuscitation by a medical control physician
b. The patient’s friend tells you that the patient does not wish to be resuscitated
c. Presence of irreversible death based on reliable criteria
d. You are presented with a valid DNAR
Answer
b. The patient’s friend tells you that the patient does not wish to be resuscitated
Rationale
C. Rationale: When delivering the shock, make sure that no one is touching the patient, including the defibrillator. Also,100% oxygen can ignite when a shock is delivered, and thus oxygen should not be flowing across the patient’s chest.
Question
You are assigned as the defibrillator on the emergency response team. While resuscitating a patient in cardiac arrest secondary to ventricular fibrillation, the team leader asks you to shock the patient. You shout, “clear! Shocking!” Which of the following is part of the assessment before delivering the shock?
a. Make sure that the bag-mask ventilation is not interrupted.
b. Support the patient while delivering the shock to ensure that the patient does not fall from the gurney.
c. Oxygen should not be flowing across the patient’s chest.
d. While delivering the shock, the defibrillator should concentrate on the monitor to ensure that an organized rhythm is achieved and the correct energy dose is delivered.
Answer
c. Oxygen should not be flowing across the patient’s chest.
Rationale
A. Rationale: It is necessary to give rescue breaths at this time to prevent hypoxemia. One breath every 6 seconds is optimal. The pulse must be checked every 2 minutes.
Question
You are assisting a patient in cardiac arrest and have assessed that the patient has a pulse but is not breathing. What is the next most important course of action?
a. Start rescue breaths, giving one breath every 6 seconds
b. Begin high-quality CPR
c. Wait for the emergency response team to arrive
d. Perform a precordial thump
Answer
a. Start rescue breaths, giving one breath every 6 seconds