ACLS Principles Flashcard 14
Rationale
B. Rationale: Return of spontaneous circulation is the goal of CPR. If this is achieved, the heart resumes a perfusing rhythm. A pulse is felt, and blood pressure is measured. Quantitative waveform capnography will demonstrate an increase in ETCO2 to 35–40 mm Hg. An ECG tracing demonstrating normal sinus rhythm may be possible in patients with cardiac arrest; this is known as pulseless electrical activity, a nonshockable cardiac arrest rhythm. The presence of lividity is a sign of irreversible death.
Question
Which one of the following clinical findings is an indication of return of spontaneous circulation?
a. ECG tracing of normal sinus rhythm
b. End-tidal CO2 of 40 mm Hg
c. Presence of lividity
d. All of the above
Answer
b. End-tidal CO2 of 40 mm Hg
Rationale
D. Rationale: Atrial fibrillation is not a cardiac arrest rhythm.
Question
Which one of the following ECG rhythms is not a cardiac arrest rhythm?
a. Ventricular fibrillation
b. Asystole
c. Pulseless electrical activity
d. Atrial fibrillation
Answer
d. Atrial fibrillation
Rationale
D. Rationale: The following are cardiac arrest rhythms: asystole, pulseless electrical activity, pulseless ventricular tachycardia, and ventricular fibrillation.
Question
Which one of the following is a cardiac arrest rhythm?
a. Third-degree AV block
b. Atrial flutter
c. Second-degree AV block
d. Ventricular fibrillation
Answer
d. Ventricular fibrillation
Rationale
D. Rationale: Cardiac arrest rhythms include asystole, pulseless electrical activity, pulseless ventricular tachycardia, and ventricular fibrillation. (ACLS Case: Cardiac Arrest)
Question
Which one of the following is a cardiac arrest rhythm?
a. Third-degree AV block
b. Atrial flutter
c. Second-degree AV block
d. Ventricular fibrillation
Answer
d. Ventricular fibrillation
Rationale
C. Rationale: Ventilations are given at a ratio of 2 ventilations every 30 chest compressions. Excessive ventilations cause increased intrathoracic pressure, which reduces venous return to the heart, leading to poor cardiac output. Hyperventilation also causes cerebral vasoconstriction, which diminishes blood perfusion to the brain.
Question
Which one of the following is a result of excessive ventilations during CPR?
a. Dilates cerebral blood vessels
b. Decreases intrathoracic pressure
c. Decreases venous return to the heart
d. Improves tissue oxygenation
Answer
c. Decreases venous return to the heart
Rationale
B. Rationale: A prerequisite for waveform capnography is that cardiac arrest patients must be intubated first with an ET tube or laryngeal mask.
Question
Which one of the following is an indication for waveform capnography?
a. All patients with cardiac arrest
b. Only intubated cardiac arrest patients
c. Cardiac arrest patients with shockable rhythms
d. Cardiac arrest patients with nonshockable rhythms
Answer
b. Only intubated cardiac arrest patients
Rationale
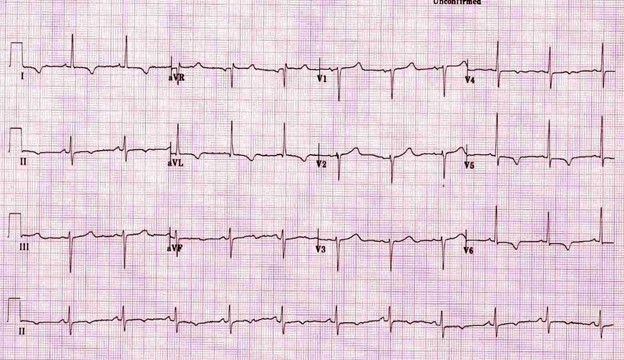
B. Rationale: Pulseless electrical activity (PEA) is a cardiac arrest rhythm described as an organized sinus rhythm in the absence of any pulse. The most common cause of pulseless electrical activity is respiratory failure. After interventions to improve respiratory failure by enhancing oxygenation and ventilation are performed along with high-quality CPR, there is a chance that PEA will convert into a perfusing rhythm.
Question
Which one of the following is described as having an organized rhythm but no pulse?
a. Ventricular fibrillation
b. Pulseless electrical activity
c. Pulseless ventricular tachycardia
d. Asystole
Answer
b. Pulseless electrical activity
Rationale
B. Rationale: As several randomized controlled trials failed to exhibit some benefit of applying transcutaneous pacing to cardiac arrest patients in asystole, and the AHA does not recommend such treatment.
Question
Which one of the following is NOT an integral part of managing cardiac arrest secondary to asystole?
a. When it is unclear that the ECG tracing is a fine ventricular fibrillation or asystole, one shock should be given.
b. Transcutaneous pacing can convert asystole into an organized rhythm.
c. Administration of bolus IV injections of epinephrine 1 mg every 3 to 5 minutes is recommended
d. High-quality CPR is the priority of treatment.
Answer
b. Transcutaneous pacing can convert asystole into an organized rhythm.
Rationale
A. Rationale: The ACLS course showcases 9 clinical conditions termed as cases in the ACLS provider manual. These clinical conditions include the following:
Respiratory arrest
Acute Coronary Syndromes
Acute Stroke
VF/pulseless VT
Asystole
Pulseless Electrical Activity (PEA)
Bradycardia
Tachycardia (Stable and Unstable)
Immediate Post-Cardiac Arrest Care
Question
Which one of the following is not included in the ACLS provider course?
a. Renal failure
b. Respiratory arrest
c. Bradycardia
d. Immediate post-cardiac arrest care
Answer
a. Renal failure
Rationale
D. Rationale: There is no need for a rapid bolus injection when administering epinephrine. This procedure is necessary for adenosine administration due to its fast half-life.
Question
Which one of the following is NOT part of the procedure when administering IV epinephrine during resuscitation?
a. Follow up IV injection of epinephrine with 20 mL saline flush
b. Elevate limb with the IV access during administration
c. Prepare 1.0 mg epinephrine (10 mL of a 1:10,000 solution)
d. Rapid bolus injection of epinephrine within 1 to 3 seconds
Answer
d. Rapid bolus injection of epinephrine within 1 to 3 seconds