Arrhythmias Flashcard 1
Rationale
B. Rationale: Emergency cardiovascular care guidelines suggest that transcutaneous pacing is probably indicated if patients with bradycardia are unresponsive to drugs.
Question
A patient who suddenly developed hypotension and chest pain with bradycardia has not improved after repeated doses of atropine and an epinephrine infusion. What other treatment should be administered to improve the patient’s condition?
a. synchronized cardioversion
b. transcutaneous pacing
c. adenosine 6 mg IV bolus
d. amiodarone 300 mg IV bolus
Answer
b. transcutaneous pacing
Rationale
C. Rationale: This patient likely has significant internal bleeding from his multiple traumatic injuries. Cardiac arrest is most likely secondary to hypovolemia from the blood loss. As this is an extracardiac problem leading to hypovolemia, he will likely have PEA. PEA is a common finding in hypoxia and hypovolemia, which are highly treatable causes of cardiac arrest. The patient will need volume resuscitation and management of any ongoing sources of bleeding. It is unlikely that a young, healthy individual will have any another cardiac arrest arrhythmia with hypovolemia as a cause for the arrest.
Question
A 17-year-old is involved in a multiple motor vehicle collision. He has multiple bony fractures, and cervical spine precautions are in place. He is unresponsive, and there are no palpable pulses. There is significant ecchymoses on his bilateral flanks and across the chest. CPR is immediately initiated. What is the most likely rhythm on cardiac monitoring?
a. Ventricular fibrillation
b. Pulseless ventricular tachycardia
c. PEA
d. Asystole
Answer
c. PEA
Rationale
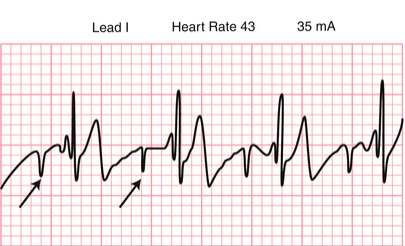
B. Rationale: This patient has hemodynamic instability from bradycardia that has failed standard therapy. TCP can be used as a temporizing mechanism. The ECG shows bradycardia with a wide QRS. The pacer spikes are noted as negative square deflections, however, there is no subsequent QRS wave with the T waves. Consequently, capture is not occurring. The initial step to manage this is to increase the pacer current to above the threshold needed to capture. Following this, adjusting the pacer pads may be necessary. It is also important to ensure there are no comorbidities interfering with capture such as intrathoracic air (pneumothorax), fluid (pericardial effusion) or severe hyperkalemia. There has been no capture, so it is unlikely the pulse will be changed. It is premature to start chest compressions when capture has not occurred, although this may be the next step if capture occurs and the patient is still pulseless. The patient does not have a shockable rhythm at this point. A large electrical artifact from the pacer can obscure a shockable rhythm. While this may be a finding if monitor blanking is not completed, ensuring capture will be the first step before looking for underlying VF. Additionally, the pulse should be checked again before defibrillation.
Question
A 43-year-old woman has significant hypotension and bradycardia. She has not improved with atropine and epinephrine. Her pulse is thready but palpable. She is being managed with transcutaneous pacing. Her ECG is below:
a. Check for a pulse
b. Increase pacer current
c. Start chest compressions
d. Provide biphasic defibrillation
Answer
b. Increase pacer current
Rationale
A. Rationale: This man likely has an AV node reentry tachycardia (or AVNRT). This can be due to an alternate conduction pathway, or it can occur in healthy individuals with stimulants or environmental factors such as caffeine, hypoxia, tachycardia, or anxiety. It can also be seen in patients with underlying cardiac or pulmonary conditions such as CAD. ECG findings of a sudden run of narrow QRS tachycardia that resolves spontaneously suggests the diagnosis. The initial symptomatic treatment is vagal stimulation or adenosine. In a patient with increasing frequency and no known stimulus, the team should assess for an underlying etiology. Amiodarone or digoxin are not the initial treatment in a mildly symptomatic patient.
Question
A 49-year-old man complains of palpitations that have become more frequent. He notes that it is worse with caffeine and exercise, although it seems now to occur even when he has not had coffee. He has no major medical problems. ECG reveals a run of narrow QRS beats with a rate of 140 bpm that suddenly terminates, with the patient in normal sinus rhythm. The symptoms recur. What is the best initial treatment?
a. Vagal stimulation
b. Amiodarone
c. Reassurance
d. Digoxin
Answer
a. Vagal stimulation
Rationale
B. Rationale: This patient likely has hyperkalemia. He has several risk factors (renal failure and medication history), signs of potassium toxicity, and ECG findings consistent with increased potassium (e.g., peaked T waves and wide QRS). While hypokalemia can also lead to weakness, the associated ECG changes are different (e.g., flattened T waves and wide QRS), and it is typically associated with GI or renal losses rather than chronic renal failure. Sodium changes (hypo- or hypernatremia) are less likely to cause such significant ECG findings. Typically, there will be more neurologic abnormalities, including confusion, irritability, and seizures. Sodium abnormalities are typically associated with total body water changes.
Question
A 55-year-old man with chronic kidney failure has increasing hypotension and paresthesias. He develops progressive weakness and respiratory failure. He takes beta-blockers and ACE inhibitors for renal protection and associated hypertension. His ECG shows peaking T waves, a wide QRS, and a prolonged QT interval. What is the likely electrolyte abnormality in this patient?
a. Hypernatremia
b. Hyperkalemia
c. Hypokalemia
d. Hyponatremia
Answer
b. Hyperkalemia
Rationale
A. Rationale: Even though the rhythm looks like sinus bradycardia, the fact that there is no pulse means that the patient is in cardiac arrest secondary to pulseless electrical activity. Rescuers must recognize this as soon as possible so that high-quality CPR can be provided immediately. (ACLS Case: Adult Cardiac Arrest: Dynamic PEA rhythm)
Question
A 65-year-old man is brought to the emergency department. The patient is unconscious with no pulse, and he is not breathing spontaneously. When an ECG is ordered, the following tracing is recorded:
What is the interpretation of this ECG finding?
a. pulseless electrical activity
b. sinus bradycardia
c. idioventricular rhythm
d. first-degree AV block
Answer
a. pulseless electrical activity
Rationale
B. Rationale: The patient has atrial fibrillation. He is at increased risk for stroke or transient ischemic attack (TIA) in the long term due to the risk of thrombus from the atrium to the cerebral circulation causing a stroke. Atrial fibrillation is associated with many underlying cardiac and pulmonary conditions, such as ACS, valvular disease, and pulmonary emboli.
Question
A 74-year-old man has the following ECG finding:
What is a significant long-term risk for this patient?

a. acute MI
b. stroke
c. cardiomyopathy
d. pulmonary emboli
Answer
b. stroke
Rationale
C. Rationale: Bradyarrhythmia’s that are unlikely to respond to atropine are second-degree AV block (Mobitz type 2) and third-degree AV block or a block of non-nodal origin.
Question
A bradyarrhythmia unlikely to respond to atropine is:
a. a first-degree AV block
b. a second degree AV block (Mobitz type 1)
c. a third-degree AV block
d. none of the above
Answer
c. a third-degree AV block
Rationale
B. Rationale: One of the important factors for successful advanced cardiac life support is the shortest time to defibrillation. When a shockable rhythm is diagnosed, then defibrillation should not be delayed.
Question
A patient with cardiac arrest secondary to pulseless ventricular tachycardia is being resuscitated. After 5 cycles of compression, the biphasic defibrillator is charged and ready to give a shock. What should the team do next?
a. Continue high-quality CPR for 2 minutes.
b. Defibrillate.
c. Insert an IV line and inject a 1 mg bolus of epinephrine IV every 3–5 minutes.
d. Intubate the patient.
Answer
b. Defibrillate.
Rationale
D. Rationale: Wide QRS tachycardia is typically assumed to originate in the ventricles, however, this is not always the case. With a left bundle branch block, a supraventricular tachycardia can appear wide due to the slowed conduction via the right bundle branch. Polymorphic wide QRS should be managed similarly to VF, with defibrillation. Adenosine is used for symptomatic tachycardias but is not used in the management of unstable wide QRS tachycardias. It can help differentiate a supraventricular from ventricular etiology. However, there is a risk of VF in this case. Verapamil should not be given to patients with ventricular tachycardias as this can precipitate hemodynamically significant hypotension.
Question
A wide QRS tachycardia:
a. Should be managed with cardioversion if polymorphic
b. Can be treated with adenosine if the patient is unstable
c. Can be managed with verapamil if originating in the ventricle.
d. Can be supraventricular when associated with a bundle branch block
Answer
d. Can be supraventricular when associated with a bundle branch block