Cardiac Arrest Flashcard 3
Rationale
B. Rationale: The patient must be intubated through the endotracheal tube to administer the drug via the endotracheal route. Instead of intravenous application of cardiac arrest drugs such as epinephrine, lidocaine, atropine, and naloxone, the drug is absorbed in the bronchial tree. Since the absorption in this region is significantly lower, the recommended dose of the drug is usually higher. For epinephrine, it is recommended a dose that is 10 times higher than the IV or IO route.
Question
The recommended endotracheal dose of epinephrine for an intubated pediatric patient in cardiac arrest is:
a. Equal to the intravenous dose
b. 10 times higher than the recommended intravenous dose
c. Half of the intravenous dose
d. Not to be given via the endotracheal route
Answer
b. 10 times higher than the recommended intravenous dose
Rationale
C. Rationale: When an advanced airway is in place, the sequence of ventilation becomes continuous and timed perfectly during chest recoil to prevent pneumothorax, known as asynchronous ventilations. The team member gives 1 breath every 2 to 3 seconds while the compressor continues to provide chest compressions at a rate of 100 to 120 per minute.
Question
The team leader gives orders to intubate a patient in cardiac arrest. When performing conventional CPR, how should the team provide ventilations and compressions when an advanced airway is in place?
a. Give 30 chest compressions then 2 ventilations
b. Give 15 chest compressions then 2 ventilations
c. Give asynchronous ventilations and continue chest compressions
d. Connect the mechanical ventilator and continue chest compressions
Answer
c. Give asynchronous ventilations and continue chest compressions
Rationale
D. Rationale: The American Heart Association Pediatric Cardiac Arrest algorithm recommends calculating the first shock dose at 2 J/kg. Subsequent doses can be calculated at 4 J/kg and more until adult doses are reached. It is recommended not to use too much energy in pediatric patients if it can be avoided. However, giving a shock when feasible is better than no shock at all. Thus, if only an adult defibrillator is available, the code team may use the adult dose for cardioverting a shockable cardiac arrest rhythm.
Question
What is the recommended first shock dose according to the American Heart Association Pediatric Cardiac Arrest algorithm?
a. 10 J/kg
b. 6 J/kg
c. 5 J/kg
d. 2 J/kg
Answer
d. 2 J/kg
Rationale
A. Rationale: A visible chest rise and limiting respiration rates to 20 to 30 per minute ensures adequate ventilation and prevents overventilation of the patient, which can increase intrathoracic pressure and reduce survival rates. A common sequela of too much ventilation is pneumothorax and volutrauma.
Question
When providing ventilations, achieving only a visible chest rise with a respiratory rate of 20 to 30 breaths per minute is enough to prevent which one of the following untoward effects of providing positive pressure ventilation?
a. Pneumothorax
b. Hypoxia
c. Myocardial infarction
d. Cheyne-stokes respiration
Answer
a. Pneumothorax
Rationale
D. Rationale: Epinephrine can be delivered through an intravenous line, intraosseous line, or an advanced airway via the endotracheal route. Absorption of the medication through the endotracheal route is greatly decreased. When the endotracheal route is used, the dose of epinephrine must be ten times higher than the IV or IO dose in order to reach its therapeutic action. Endotracheal delivery of epinephrine should only be done while the team works to get IV or IO access.
Question
Which are possible routes of administration of epinephrine?
a. Intravenous
b. Intraosseous
c. Endotracheal
d. All of the above
Answer
d. All of the above
Rationale
C. Rationale: Choice A is ventricular fibrillation, choice B is pulseless ventricular tachycardia, and choice C is asystole. Asystole and pulseless electrical activity are non shockable rhythms. Ventricular fibrillation and pulseless ventricular tachycardia are shockable rhythms. High quality CPR without defibrillation is necessary if the rhythm is a non shockable rhythm such as asystole or pulseless electrical activity. The patient should be closely monitored for rhythm changes.
Question
Which of the following cardiac arrest rhythms is a non shockable rhythm?
a. Ventricular fibrillation
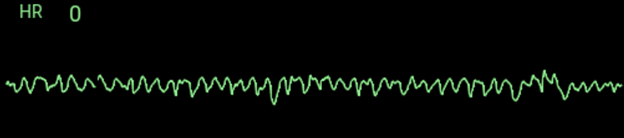
b. Pulseless ventricular tachycardia
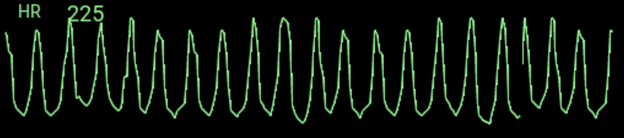
c. Asystole

d. All of the above are non-shockable rhythms
Answer
c. Asystole

Rationale
A. Rationale: There are two pathways of cardiac arrest, the hypoxic arrest pathway, and the sudden cardiac arrest pathway. The hypoxic arrest results in tissue hypoxia and acidosis. It is more common in infants and children and is the result of respiratory failure or hypotensive shock. The precipitating medical problem likely caused cardiopulmonary failure, which then progressed to cardiac arrest. Acute respiratory distress syndrome is a medical condition in which widespread pulmonary inflammation has occurred in a critically ill patient. Sudden infant death syndrome (SIDS) is seen in babies less than 12 months of age that have died during sleep without any warning signs.
Question
Which of the following is a pathway of cardiac arrest?
a. Hypoxic arrest
b. Acute respiratory distress syndrome
c. Sudden infant death syndrome
d. Asystole
Answer
a. Hypoxic arrest
Rationale
D. Rationale: Hypoxic arrest is a medical condition brought about by shock or respiratory failure. These are the most common causes of cardiac arrest in infants and children, and management must be planned to correct these two conditions to prevent the pediatric patient from progressing into cardiac arrest.
Question
Which of the following medical conditions can cause hypoxic arrest?
a. Hypovolemic shock
b. Respiratory arrest
c. Anaphylactic shock
d. All of the above
Answer
d. All of the above
Rationale
B. Rationale: If the patient is in the ICU, the team members may have the luxury of monitoring physiologic measurements such as the end-tidal CO2 (ETCO2). ETCO2 can give the resuscitation team an idea of the effectiveness and quality of chest compressions. An ETCO2 < 10–15 mm Hg means that there is inadequate cardiac output, and chest compressions must be improved. Chest compression-induced stroke volume and cardiac output can be monitored with an indwelling arterial catheter, using the waveform as a guide. Poor waveforms are produced if the hand positioning is wrong, which should signal the provider to adjust. ETCO2 and arterial waveform can be used to monitor for return of spontaneous circulation.
Question
While performing CPR in a pediatric ICU setting, an end-tidal carbon dioxide reading < 15 mm Hg indicates:
a. Good cardiac output
b. Poor quality chest compressions
c. Poor arterial oxygen saturation
d. Return of spontaneous circulation
Answer
b. Poor quality chest compressions
Rationale
C. Rationale: Team members must call for assistance as soon as possible, rather than waiting until they collapse or the patient deteriorates. Do not reject offers from others to carry out a task that you are unable to perform. Team members should rotate tasks to prevent fatigue.
Question
While performing CPR on a 6-year-old boy in the ICU, you notice that your triceps are cramping up on the third cycle of CPR. What should you do in this situation?
a. Continue CPR until the 5th cycle, then request assistance
b. Stop CPR and stretch the muscle to relieve the pain
c. Tell your team leader right away so that you can be replaced
d. Do not let your teammates interrupt what they are doing to assist you
Answer
c. Tell your team leader right away so that you can be replaced