Stroke Flashcard 3
Rationale
A. Rationale: Time zero is when the patient was last known to be normal (i.e., symptom-free). If the patient wakes from sleep with stroke symptoms, time zero is the last time anyone saw the patient without symptoms.
Question
For a patient with stroke, time zero is:
A. When the patient was last known to be normal
B. When the patient enters the ED
C. When EMS is dispatched to see the patient
D. When the patient is first assessed by the stoke team
Answer
A. When the patient was last known to be normal
Rationale
C. Rationale: The maximum time for administration of fibrinolytic therapy from ED arrival is within 60 minutes.
Question
For patients with ischemic stroke, in what timeframe from hospital arrival should fibrinolytic therapy be administered?
a. 15 minutes
b. 30 minutes
c. 1 hour
d. 3 hours
Answer
c. 1 hour
Rationale
C. Rationale: A facility without appropriate systems to care for the patient should transfer the patient to another hospital with a dedicated stroke unit. Assessing the patient with suspected stroke should be performed by an experienced provider within 10 minutes of arrival in the ED, but this is not a foundational fact. The receiving hospital should detail the roles of healthcare providers in the care of patients with acute stroke, including identifying sources of neurologic expertise.
Question
Foundational facts in acute stroke care include:
a. Detailing healthcare provider roles in the care of patients with a bleeding diathesis
b. Assessing the patient with suspected stroke within 30 minutes of arrival in the ED
c. Transferring the patient to another hospital with a dedicated stroke unit when appropriate
d. All of the above
Answer
c. Transferring the patient to another hospital with a dedicated stroke unit when appropriate
Rationale
A. Rationale: A CT scan of the head is the most important test to determine the use of fibrinolytic therapy in acute stroke because it can ascertain its cause as ischemic vs. hemorrhagic. (ACLS Case: Acute Stroke)
Question
Healthcare providers must immediately treat a stroke patient in the ED to prevent the patient from deteriorating. What is the most important test to determine the use of fibrinolytic therapy in acute stroke?
a. CT scan of the head
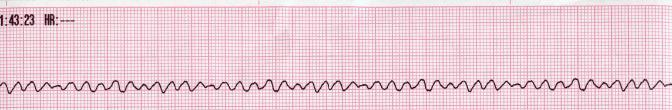
b. ECG
c. Doppler ultrasound
d. Chest X-ray
Answer
a. CT scan of the head
Rationale
B. Rationale: Blood glucose levels must be monitored in patients with acute stroke because hyperglycemia is correlated with worsening outcomes. If the blood glucose level is above 185 mg/dL, it is recommended that these patients be given insulin to control their serum glucose.
Question
Hyperglycemia in acute stroke is associated with a worsening clinical outcome. At what upper limit of blood glucose level should healthcare providers consider insulin therapy?
a. Above 120 mg/dL
b. Above 185 mg/dL
c. Above 220 mg/dL
d. Above 250 mg/dL
Answer
b. Above 185 mg/dL
Rationale
A. Rationale: The extended window for treating carefully selected patients with acute ischemic stroke with IV rtPA is 3.0–4.5 hours. Anticoagulants or antiplatelet therapy should not be given for 24 hours after rtPA is administered.
Question
If a patient with stroke remains a candidate for thrombolytic therapy after passing the relative exclusion criteria:
a. Discuss relative risks or benefits with the patient or family members.
b. Proceed with rtPA if the patient’s symptom onset was within 6 hours.
c. Begin anticoagulant therapy.
d. All of the above.
Answer
a. Discuss relative risks or benefits with the patient or family members.
Rationale
E. Rationale: Routine use of oxygen is only indicated if the patient is hypoxemic.
Question
Immediate general assessment and stabilization of the patient with a suspected stroke include:
a. Administering oxygen
b. Emergent CT scan or MRI of the brain
c. Performing a neurologic screening assessment
d. All of the above
e. B and C
Answer
e. B and C
Rationale
B. Rationale: If the patient’s neurologic deficits are rapidly improving or if there is evidence of hemorrhage, the patient is not a candidate for rTPA.
Question
In a patient with stroke, rTPA is indicated if:
a. Deficits are rapidly improving.
b. No anticoagulant therapy has been given for 24 hours.
c. The hemorrhage is small.
d. All of the above
Answer
b. No anticoagulant therapy has been given for 24 hours.
Rationale
A. Rationale: EMS providers should identify signs and establish time of onset. They provide supplementary oxygen if the patient is hypoxemic (SpO2 < 94%). Time of onset is the time the patient was last known to be without stroke symptoms.
Question
In cases of suspected stroke, prehospital EMS providers:
a. Establish time of symptom onset
b. Begin time zero when the patient awakens from sleep with symptoms of a stroke
c. Do not provide supplementary oxygen until patient has been assessed by a physician
d. All of the above
Answer
a. Establish time of symptom onset
Rationale
A. Rationale: However, treatment should be discontinued with a platelet count < 100,000/mcL.
Question
In patients without a history of thrombocytopenia, treatment with rtPA can be initiated before availability of the platelet count.
a. True
b. False
Answer
a. True