Assessment Flashcard 3
Rationale
C. Rationale: A patient in cardiac arrest secondary to severe accidental hypothermia that has achieved ROSC may be treated with target temperature management with a temperature goal of 32–34°C (89.6–93.2°F).
Question
A patient in cardiac arrest secondary to severe hypothermia has achieved return of spontaneous circulation. At what targeted temperature should the patient be maintained, provided that there are no contraindications?
a. Below 28°C (82.4°F)
b. 28–30°C (82.4–86°F)
c. 32–34°C (89.6–93.2°F)
d. Above 34°C (93.2°F)
Answer
c. 32–34°C (89.6–93.2°F)
Rationale
B. Rationale: A systolic BP < 90 mm Hg is a vital sign in the red zone and will require a house officer review within 20 minutes.
Question
A patient in the general wards is symptomatic with a BP of 70/40 mm Hg. What is the next action?
a. Call for medical emergency team
b. House officer review within 20 minutes
c. Begin CPR
d. No change in management necessary
Answer
b. House officer review within 20 minutes
Rationale
B. Rationale: The normal GRW is 1.3, and this value decreases with brain edema. A marked reduction of the GWR obtained by CT scan taken within 2 hours after cardiac arrest predicts a poor neurologic outcome.
Question
A patient is comatose after a car crash. The neurosurgeon wants to find out if the patient has brain edema using a noninvasive imaging modality. Brain edema is represented by the gray-white ratio (GWR) on CT Scan. The normal GWR value is:
a. 1.0
b. 1.3
c. 1.6
d. 2.0
Answer
b. 1.3
Rationale
D. Rationale: A red zone patient should be managed with a house officer review within 20 minutes, consideration for an ICU referral, informing the nurse in charge, and increasing the frequency of vital signs monitoring.
Question
A patient whose Early Warning Score is in the red zone should receive which intervention?
a. Increased frequency of monitoring
b. Consideration for an ICU referral
c. House officer review within 20 minutes
d. All of the above
Answer
d. All of the above
Rationale
A. Rationale: Brain CT scan can detect brain edema, which is an indication of a poor neurologic outcome.
Question
A patient with a head injury from a vehicular crash was revived after cardiopulmonary resuscitation but is in a coma. CT scan findings reveal brain edema. What is the likely outcome for this patient with a traumatic brain injury?
a. Brain edema is an indicator of poor neurologic outcome.
b. Brain edema is a sign of early neurologic recovery.
c. Brain edema is an unremarkable finding in comatose patients.
d. Brain edema is a sign of intracranial hemorrhage that must be evacuated at once.
Answer
a. Brain edema is an indicator of poor neurologic outcome.
Rationale
A. Rationale: Hypovolemia is a reversible cause of cardiac arrest, and pulseless electrical activity is a common associated finding. The usual ECG morphology is a narrow complex tachycardia, but since the patient is in cardiac arrest, the diagnosis is pulseless electrical activity. The treatment is to provide the patient with volume replacement and ACLS. Pulseless electrical activity is a nonshockable rhythm.
Question
A patient with a stab wound is brought to the emergency department. He is nonresponsive and has no spontaneous breathing. You are unable to detect a pulse, but the ECG tracing records the following finding:
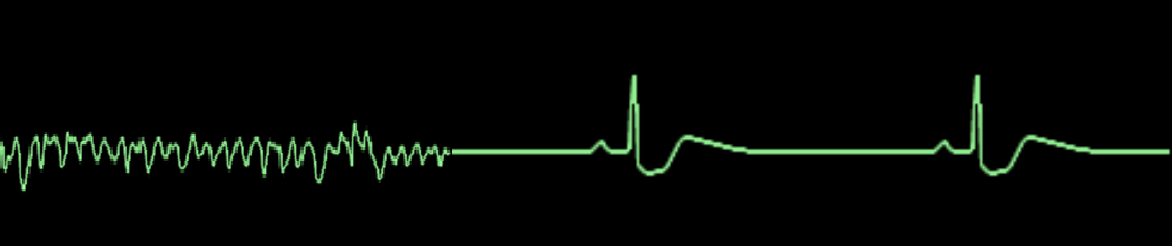
What is your interpretation of this ECG finding?
a. Pulseless electrical activity
b. Narrow complex tachycardia
c. Ventricular tachycardia
d. Atrial fibrillation
Answer
a. Pulseless electrical
Rationale
D. Rationale: A patient with a vital sign in the EWS yellow zone can be treated by managing pain, fever, or distress and increasing the frequency of vital sign monitoring.
Question
A patient with a vital sign in the Early Warning Score yellow zone can be:
a. Given acetaminophen
b. Given PRN pain medication
c. Monitored more frequently
d. All of the above
Answer
d. All of the above
Rationale
C. Rationale: A patient with an EWS of 8–9 is in the red zone and likely to deteriorate rapidly.
Question
A patient with an Early Warning Score of 9:
a. Has unstable chronic disease
b. Is likely to deteriorate rapidly
c. Has an immediately life-threatening critical illness
d. None of the above
Answer
c. Has an immediately life-threatening critical illness
Rationale
A. Rationale: An oxygen saturation ≥ 96% is normal and will not require any intervention.
Question
A patient with an oxygen saturation of 96% will require what mandatory action?
a. No intervention is necessary
b. Increase in frequency of vital signs monitoring
c. Inform the house officer
d. Inform the registrar
Answer
a. No intervention is necessary
Rationale
C. Rationale: In the clinical scenario of a bee sting with orbital edema and tachypnea, the patient’s stridor is likely due to a swollen epiglottis or tongue. The symptoms indicate the patient is trying to maintain adequate gas exchange despite this airway obstruction and is in respiratory distress.
Question
A patient you are seeing in the emergency department was stung by a bee. He has periorbital edema with nasal flaring and supraclavicular retractions. You note that he is tachypneic with stridor and diagnose anaphylaxis. Of the following, which one best describes the patient’s clinical condition from a respiratory standpoint?
a. Respiratory compensation
b. Respiratory failure
c. Respiratory arrest
d. Respiratory distress
Answer
c. Respiratory arrest