Arrhythmias Flashcard 10
Rationale
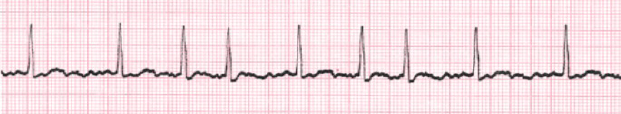
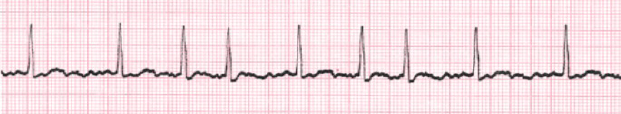
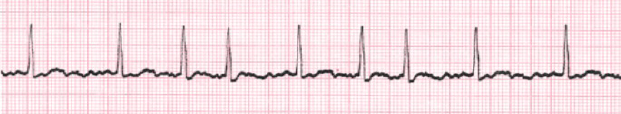
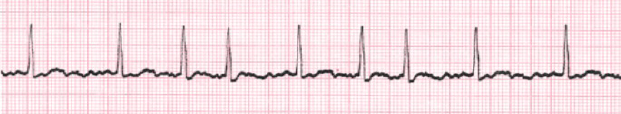
C. Rationale: Sinus bradycardia is a rhythm that has fewer than the normal number of impulses arising from the sinoatrial node at a rate of < 50 bpm.
Question
Which one of the following best describes sinus bradycardia?
a. Heart rate > 100 bpm
b. Heart rate between 60 and 100 bpm
c. Heart rate < 50 bpm
d. An irregularly irregular heart rate > 200 bpm
Answer
c. Heart rate < 50 bpm
Rationale
D. Rationale: The vital decision point in managing bradyarrhythmia is determining whether a patient is stable or unstable. Patients with symptomatic bradyarrhythmia’s will have symptoms such as palpitations, dyspnea, and light-headedness. Unstable patients will show these symptoms plus altered sensorium; compromised perfusion, oxygenation, and ventilation; and shock. The presence of unstable symptoms means that cardiac arrest is imminent.
Question
Which one of the following clinical signs or symptoms in patients with bradyarrhythmia will cause them to be diagnosed as unstable?
a. Dyspnea
b. Palpitations
c. Light-headedness
d. Altered mental status
Answer
d. Altered mental status
Rationale
B. Rationale: Bradycardia may be caused by antiarrhythmics (quinidine and amiodarone) and antihypertensive agents (methyldopa).
Question
Which one of the following drugs does NOT cause bradycardia?
a. Quinidine
b. Levothyroxine
c. Methyldopa
d. Amiodarone
Answer
b. Levothyroxine
Rationale
A. Rationale: AV nodal blocking agents (i.e., beta-blockers, calcium channel blockers, digoxin, adenosine) should be avoided in patients with an irregular wide complex tachycardia. If the rhythm is pre-excited atrial fibrillation, these drugs may cause a paradoxical increase in the heart rate (ventricular response).
Question
Which one of the following drugs should be avoided in patients with an irregular wide complex tachycardia?
A. Adenosine
B. Amiodarone
C. Lidocaine
D. Procainamide
Answer
A. Adenosine
Rationale
C. Rationale: The Valsalva maneuver is one of the vagal maneuvers that make up the preferred initial management of paroxysmal supraventricular tachycardia (PSVT). The effect of these maneuvers is temporary unless the underlying cause of PSVT is treated.
Question
Which one of the following is a vagal maneuver?
a. Trendelenburg
b. Dix Hallpike
c. Valsalva
d. Stimson
Answer
c. Valsalva
Rationale
C. Rationale: Adenosine can terminate wide-complex tachyarrhythmias only if the ECG tracing is regular and monomorphic.
Question
Which one of the following is a wide QRS complex tachyarrhythmia that can be treated with adenosine?
a. All wide QRS complex tachyarrhythmias can be treated with adenosine.
b. Adenosine is contraindicated in all wide QRS complex tachyarrhythmias.
c. Adenosine can be used in regular and monomorphic tachyarrhythmias.
d. Adenosine can only be used in pulseless wide QRS complex tachyarrhythmias.
Answer
c. Adenosine can be used in regular and monomorphic tachyarrhythmias.
Rationale
A. Rationale: Emergency cardiovascular care guidelines suggest that atropine remains the first-line drug treatment for acute symptomatic bradycardia. Transcutaneous pacing and dopamine may be used if atropine is not effective. (ACLS Case: Symptomatic Bradycardia)
Question
Which one of the following is NOT a treatment for bradycardia?
a. Adenosine
b. Atropine
c. Transcutaneous pacing
d. Dopamine
Answer
a. Adenosine
Rationale
B. Rationale: Synchronized cardioversion is the mainstay of treatment for unstable patients that have tachyarrhythmias with a pulse.
Question
Which one of the following is not part of the treatment for stable asymptomatic supraventricular tachycardia?
a. Vagal maneuvers
b. Cardioversion
c. Beta-blockers
d. Adenosine
Answer
b. Cardioversion
Rationale
B. Rationale: In recent studies, lidocaine has now become a second-line antiarrhythmic therapy for monomorphic ventricular tachycardia.
Question
Which one of the following is the least effective drug in terminating hemodynamically stable sustained ventricular tachycardia?
a. Amiodarone
b. Lidocaine
c. Procainamide
d. Sotalol
Answer
b. Lidocaine
Rationale
A. Rationale: Cardiac output is caused by myocardial contractility and heart rate. Heart rate is severely compromised in symptomatic bradyarrhythmia, and the hypoxemia in these patients is caused by ineffective cardiac output.
Question
Which one of the following pathophysiologic effects of bradyarrhythmia will cause the patient to show signs and symptoms of hypoxemia?
a. Ineffective cardiac output
b. Increase preload
c. Depressed afterload
d. Poor ventilation
Answer
a. Ineffective cardiac output