Arrhythmias Flashcard 2
Rationale
D. Rationale: The patient has an ST elevation myocardial infarction (STEMI) that may have affected the SA node, causing bradycardia. Immediate percutaneous coronary intervention is necessary to treat the underlying cause of bradycardia. However, to stabilize the patient, atropine is needed to increase her heart rate and blood pressure. Metoprolol is part of the treatment regimen for STEMI, but it is not given to patients with bradycardia.
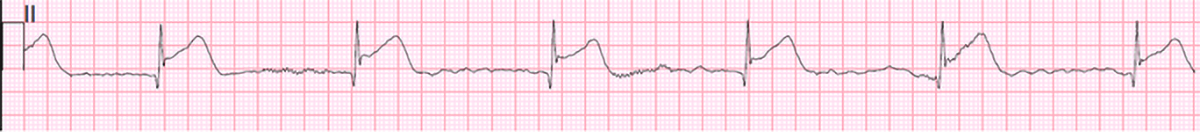
Tip: One can calculate the rate in this rhythm strip:
Rate = 60 ÷ RR interval (seconds)
In between two R-R waves, we count 7 to 8 big boxes. Conventional ECG tracings record each big box equal to 0.2 seconds. An R-R interval of 7 big boxes is equal to 1.4 seconds. Therefore, Rate = 60/1.4 or about 43 bpm. The patient has bradycardia.
Question
A 62-year-old woman is seen in the emergency department and reports crushing chest pain. She tells you that she is likely to die from it. You obtain a 12-lead ECG and find the following tracing on the 6-second strip of lead II:
What is the most appropriate treatment to address the problem in this patient?
a. Oral metoprolol 50 mg tablet
b. Adenosine 6 mg IV bolus
c. Transcutaneous pacing
d. Atropine 1 mg IV bolus
Answer
d. Atropine 1 mg IV bolus
Rationale
C. Rationale: The patient’s signs and symptoms point to instability. The patient is short of breath and complains of dizziness and palpitations. His blood pressure is low and peripheral pulses are weak. Patients with a tachyarrhythmia causing significant signs and symptoms should be sedated (if possible) and cardioverted. Patients with a narrow complex tachycardia may be given adenosine and cardioverted if adenosine is ineffective in converting the rhythm. Defibrillation should never be performed on a patient with a pulse.
Question
A 67-year-old patient is brought in by ambulance. His chief complaint is shortness of breath, dizziness, and palpitations. The paramedics report that the patient’s heart rate has been 160–180 bpm and regular. He is placed on the cardiac monitor: his oxygen saturation is 92% on room air, his BP is 88/54 mm Hg, and his heart rate is 176 bpm and regular. The monitor shows a regular wide-complex tachycardia. Peripheral pulses are weak. Oxygen is administered to maintain the patient’s oxygen saturation at ≥ 94%. Intravenous access is established. What is the next intervention?
A. Administer adenosine 6 mg rapid IV, followed by a 20 mL bolus of IV fluids.
B. Immediately defibrillate at 360 Joules for a monophasic defibrillator or 120–200 Joules for a biphasic defibrillator.
C. Consider sedation and cardiovert the patient.
D. Monitor the patient and request expert consultation.
Answer
C. Consider sedation and cardiovert the patient.
Rationale
C. Rationale: Treatment is not indicated in patients with bradycardia who are asymptomatic.
Question
A patient arrives at the clinic for a routine physical check-up and has no clinical complaints. You take her vital signs and find that she has a heart rate of 50 bpm. What is the most appropriate treatment?
a. Have the patient climb some stairs
b. Give a bolus injection of atropine 0.5 mg
c. Assure the patient that no treatment is needed
d. Give a bolus of amiodarone 300 mg IV
Answer
c. Assure the patient that no treatment is needed
Rationale
C. Rationale: Pacing should be initiated in unstable patients who do not respond to atropine. Epinephrine and dopamine are both chronotropes and vasoconstrictors. Either of these drugs may be used as an alternative to pacing when atropine fails.
Question
A patient has third-degree heart block. He reports chest pain and is hypotensive and diaphoretic. He also has pulmonary congestion. A large-bore IV has been placed in his left antecubital fossa. He has been given atropine 1 mg intravenously x 3 with only a transient increase in heart rate and no improvement of symptoms. The next intervention should be:
A. Start a dopamine infusion at 2–10 mcg/kg/min
B. Start an epinephrine infusion at 2–10 mcg/min
C. Attempt transcutaneous pacing
D. Any of these are acceptable interventions when atropine is ineffective
Answer
C. Attempt transcutaneous pacing
Rationale
A. Rationale: The ECG represents a paroxysmal supraventricular tachycardia. The QRS complexes are narrow and regular. This is a tachyarrhythmia with a pulse in a stable patient. The treatment of choice is adenosine 6 mg rapid IV push.
Question
A patient in the ED complains of palpitations. He is coherent and ambulatory. You record the following ECG tracing:
What is the first-line treatment of choice?
a. Adenosine 6 mg IV bolus injection
b. Amiodarone 300 mg IV bolus injection
c. Synchronized cardioversion 50 J after sedating the patient
d. Perform precordial thump
Answer
a. Adenosine 6 mg IV bolus injection
Rationale
C. Rationale: Synchronized cardioversion is performed in unstable narrow QRS-complex tachycardia. Adenosine would be used if the patient had a regular narrow QRS complex tachycardia, but this is not the case.
Question
A patient in the emergency department presents with a heart rate of 190 bpm, systolic blood pressure of 70 mm Hg and palpable, and is incoherent when talked to. Her ECG tracing reveals an irregular narrow-complex supraventricular tachycardia. What is the treatment of choice in this case?

a. Adenosine
b. Vagal maneuvers
c. Synchronized cardioversion
d. All of the above
Answer
c. Synchronized cardioversion
Rationale
A. Rationale: Epinephrine is not only a drug of cardiac arrest but can also be used where a vasopressor is needed, as in this case.
Question
A patient is being treated for symptomatic bradycardia. After administering the maximum dosage of atropine and initiating transcutaneous pacing, the patient has not improved. What pharmacologic treatment can help this patient?
a. Epinephrine infusion 10 mcg/min
b. Amiodarone 300 mg IV bolus
c. Sotalol 100 mg IV injection over 1 minute
d. Adenosine 6 mg rapid IV push over 3 seconds
Answer
a. Epinephrine infusion 10 mcg/min
Rationale
A. Rationale: Severe hypovolemia is often associated with a rapid and narrow complex rhythm on the monitor but no palpable pulse. The heart is empty due to inadequate preload, and there is not enough volume for the ventricle to eject. In this case, the patient may have lost a large amount of blood after the motor vehicle collision. IV fluids and blood would be required to replenish volume.
Question
A patient is in PEA. The rhythm on the monitor is narrow complex and rapid. The patient has been involved in a motor vehicle collision. Based on this information, you might suspect:
A. Hypovolemia
B. Hypokalemia
C. Hypoxia
D. Massive MI
Answer
A. Hypovolemia
Rationale
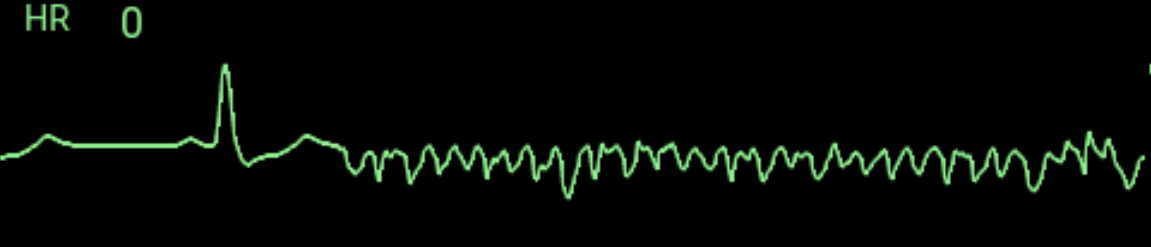
C. Rationale: The patient has atrial flutter. A narrow QRS-complex indicates that the irritable focus is supraventricular. Notice the characteristic sawtooth appearance between the QRS-complexes, which is brought about by a reentrant circuit causing a repeated loop of electrical activity that depolarizes the atrium.
Question
A patient on a cardiac monitor in the emergency department has the following tracing:
What is your diagnosis?
a. Supraventricular tachycardia
b. Ventricular tachycardia
c. Atrial flutter
d. Atrial fibrillation
Answer
c. Atrial flutter
Rationale
A. Rationale: In atrial fibrillation, the heart rate is variable with an irregularly irregular rhythm. The QRS complex is narrow and positive. Fibrillatory waves are seen in this ECG strip in place of the P waves, which have no relationship with the QRS complexes.
Question
A patient passed out when she learned that she passed the SATs with flying colors. After recovering, she is brought emergency department by her parents. She has the following ECG tracing:
What is your interpretation of this ECG finding?
a. Atrial fibrillation
b. Atrial flutter
c. Narrow complex tachycardia
d. Atrial tachycardia
Answer
a. Atrial fibrillation