Respiratory Drugs: Part 1
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
- Some common respiratory drugs are albuterol, tiotropium bromide, fluticasone, levofloxacin, and theophylline.
- Respiratory inhalers include rescue inhalers and maintenance inhalers.
- Read on to learn how each drug works, their side effects, and other essential information.
Since there are several respiratory drugs, this topic will be addressed in two articles. Part one will discuss albuterol, tiotropium bromide, fluticasone, and theophylline.Introduction to Respiratory Drugs
Albuterol is a beta2-agonist (β2-agonist). That means it acts directly on the beta-adrenergic receptors, specifically in the bronchial epithelium, causing the bronchial epithelium to dilate. Albuterol is a powerful and fast-acting bronchodilator. Albuterol is a rescue inhaler. It is important to understand how beta-blockers and beta-agonists work. The word agonist means it is potentiating, or helping, the effect. Blocker means it is stopping the reaction from happening. So, what do beta-blockers do in the body? First, they slow down the heart rate. They block sympathetic nervous system stimulation to the beta receptors on the heart, which slows the heart rate. However, bronchoconstriction can also occur, which is why providers must be cautious when administering beta-blockers to patients with asthma or chronic obstructive pulmonary disease (COPD). A beta-agonist has the opposite effect. Where beta-blockers slow the heart rate, the beta-agonist will speed it up. Likewise, a beta-agonist will bronchodilate, not Bronchoconstrict, as seen with beta-blockers. That is why albuterol is used for patients with asthma and COPD. Albuterol is a rescue inhaler. For a patient with asthma or COPD experiencing an acute episode of bronchospasm or bronchoconstriction or low oxygen saturation, albuterol is the drug of choice because it acts within 10–15 minutes. Side effects of albuterol are typically tachycardia, diaphoresis, tremor, and anxiety. Another possible side effect is hypokalemia. Where beta-blockers can increase potassium levels because they block the effects of aldosterone, the exact opposite could happen with beta-agonists, including albuterol. Patients are monitored for dysrhythmias, which could indicate a state of hypokalemia.Albuterol
Related Video – How to Manage Respiratory Arrest on an Adult
Tiotropium bromide is also a bronchodilator. It is an anticholinergic drug. It is a once-daily inhaler, also known as a maintenance inhaler. It takes a while for the bronchodilation effects to set in. Tiotropium bromide is not a rescue inhaler. Therefore, it is not the drug of choice in an emergency where the patient is unstable. Tiotropium bromide is a once-daily maintenance inhaler. The bronchodilation effects of tiotropium bromide are great for patients with COPD or chronic bronchitis, and the anticholinergic effects are excellent for patients with chronic bronchitis. In chronic bronchitis, the goblet cells are irritated and begin producing plentiful mucus, which causes a productive cough. The anticholinergic effects of tiotropium bromide decrease mucus production and help clear the airways. When taking tiotropium bromide, patients often report anticholinergic side effects, such as dry mouth, dry eyes, constipation, and possibly urinary retention. Tiotropium bromide must be used with caution in patients with glaucoma, as it can increase intraocular pressure. Read: Respiratory Drugs: Part 2Tiotropium Bromide

Next is fluticasone. Fluticasone is a corticosteroid inhaler. Any inhaler that ends in “-sone,” like dexamethasone, is a corticosteroid inhaler. Corticosteroids have very powerful anti-inflammatory effects. The steroid is great for treating inflammation, but it is not a rescue inhaler. The corticosteroid inhaler is a maintenance inhaler that is usually taken once daily. Corticosteroid maintenance inhalers are usually dosed once daily. Fluticasone is steroid. Steroids, more specifically, glucocorticoids of the corticosteroids, increase glucose because they oppose insulin in the body. The increased glucose can accumulate in the patient’s mouth and cause thrush. Patients need to be educated to rinse their mouths after using any steroid inhaler to lower the risk of developing thrush. If a patient with COPD or chronic bronchitis is prescribed all three of these inhalers, they must be administered in the order presented: albuterol first, tiotropium bromide second, and finally fluticasone. Albuterol is used first because it opens the airways. Once open, the airways are ready to receive the rest of the medications. Providers must keep in mind that it takes about 15 minutes for the albuterol to act. Next, the tiotropium bromide is administered. Finally, the fluticasone. It is given last because the patient needs to rinse their mouth after taking it.Fluticasone

Levofloxacin is a fluoroquinolone, an antibiotic. Why is an antibiotic included with respiratory drugs? Levofloxacin, along with any of the fluoroquinolones, is reserved for patients with severe respiratory infections, such as pneumonia or a COPD exacerbation, often caused by a bacterial infection. Fluoroquinolones, and levofloxacin, in particular, are reserved for patients who are very sick and have serious bacterial infections because the fluoroquinolones have serious side effects. One of the side effects is Achilles tendon rupture. If a patient on levofloxacin or another fluoroquinolone reports achy muscles in their calves, they may be experiencing an Achilles tendon rupture. Levofloxacin is also hepatotoxic. It can exacerbate myasthenia gravis, so it should not be used in patients presenting as such. In general, levofloxacin and fluoroquinolones are often only used for serious respiratory infections, such as pneumonia or COPD exacerbation with infection.Levofloxacin
Related Video – Respiratory Drugs – Part 2
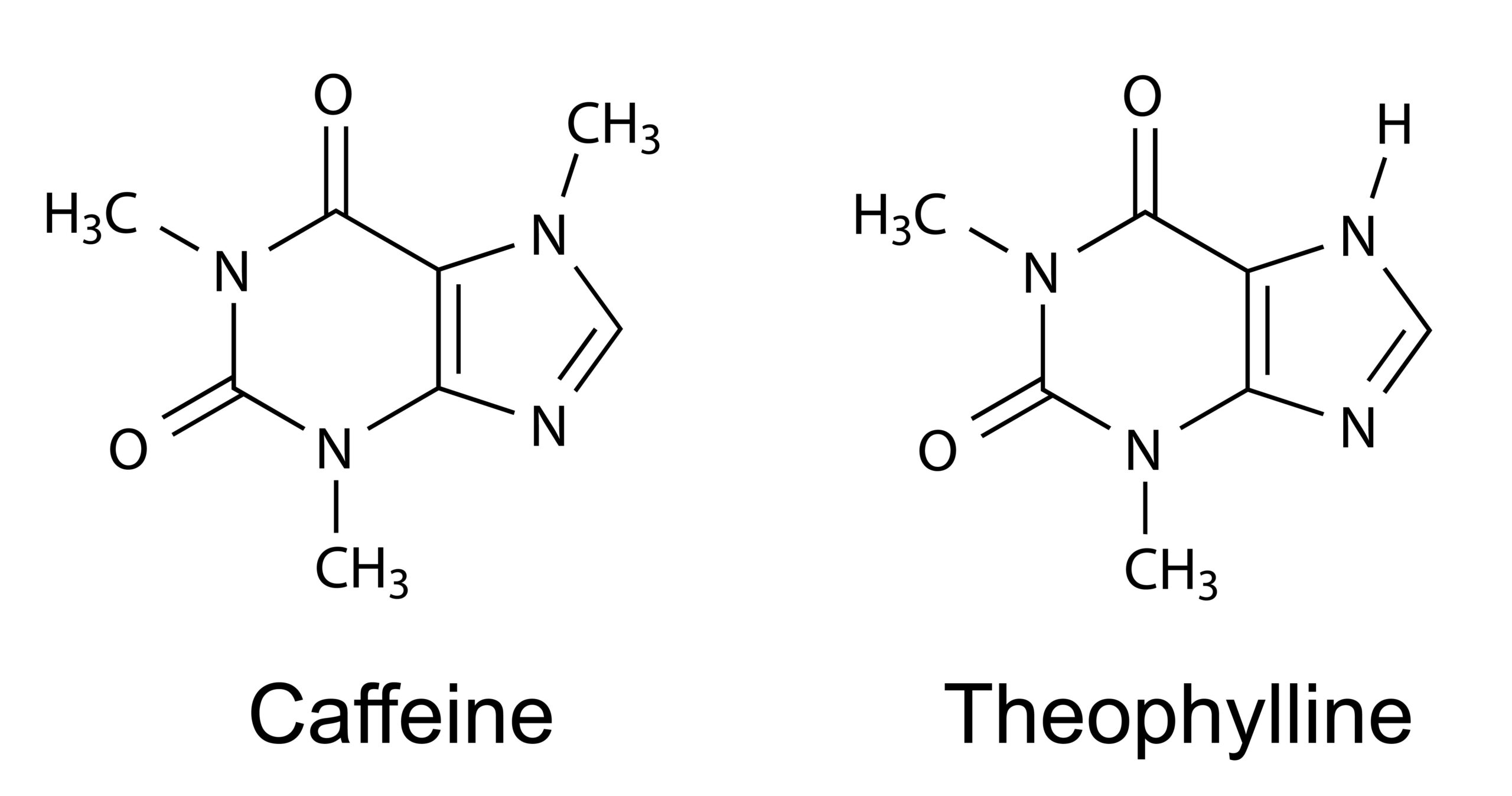
Theophylline belongs to a class of medications called xanthine’s. What is interesting about this class of medications is that xanthine’s act like caffeine, including having similar side effects. However, theophylline is a bronchodilator, similar to albuterol. Theophylline is an oral medication, not an inhaler. Theophylline and caffeine are similar compounds. Both drugs have similar side effects. Theophylline has several mechanisms of action. One, it inhibits phosphodiesterase. Inhibiting phosphodiesterase causes a cell signaling cascade that ultimately reduces inflammation. It reduces the lung’s responsiveness to irritants. It is excellent for asthma patients who have specific triggers. Theophylline also blocks adenosine receptors. Adenosine normally acts like a “heart block” and decreases conduction through the AV node. When the effects of adenosine are blocked, then the side effects of the drug are increased. The most common side effects of theophylline are increased heart rate, restlessness, nervousness, anxiety, tachycardia, and diaphoresis. These are the same side effects associated with caffeine. Theophylline is still widely used for patients with COPD because it is inexpensive and accessible. However, patients on long-term theophylline need to have their serum levels monitored regularly because theophylline toxicity can cause seizures and severe hypotension. The typical side effects of theophylline are gastrointestinal (GI) irritation, and diarrhea. These may present upon use. However, theophylline levels can reach toxic levels over time, which is why serum levels need to be monitored closely. It is important to know the different respiratory drugs, how they work, and what side effects to watch for. This article introduced some common respiratory drugs: albuterol, tiotropium bromide, fluticasone, levofloxacin, and theophylline. More will be discussed in part two.Theophylline
More Free Resources to Keep You at Your Best
Editorial Note
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.