Assessment Flashcard 1
Rationale
B. Rationale: EWS of 7 falls under the Orange Zone, which would trigger a mandatory house officer review within 60 minutes.
Question
A member of the nursing staff sees a patient with a calculated Early Warning Score of 7. What should be the next action?
a. Call for the medical emergency team
b. House officer review within 60 minutes
c. Consider ICU referral
d. Begin CPR
Answer
b. House officer review within 60 minutes
Rationale
D. Rationale: The assessment of a patient with suspected cardiac arrest is divided into three categories: (1) the BLS assessment, (2) the primary assessment, and (3) the secondary assessment.
Question
The assessment of a patient with suspected cardiac arrest is divided into which three assessment categories?
a. Untrained, trained, health professional
b. BLS, ACLS, and post-resuscitation
c. Primary, secondary, and tertiary
d. BLS, primary, and secondary
Answer
d. BLS, primary, and secondary
Rationale
C. Rationale: Isotonic solutions such as 0.9% normal saline and lactated Ringer solutions are initially the fluids of choice in restoring extracellular fluid volume in patients with severe hypovolemia secondary to trauma. D5W must be avoided because it can reduce serum sodium levels too rapidly.
Question
A 19-year-old man is brought to the emergency department in cardiac arrest secondary to perfuse bleeding from a gunshot wound. Which one of the following is the treatment of choice for this patient?
a. Norepinephrine
b. Dextrose 5% in water
c. Lactated ringer solution
d. Epinephrine
Answer
c. Lactated ringer solution
Rationale
A. Rationale: Emergency department thoracotomy can be used to clear intrapericardial fluid secondary to trauma, particularly if there are large volumes of clotted blood. Immediately after intrapericardial fluid is cleared, the heart will start contracting normally, improving circulation. Pericardiocentesis, due to the small caliber of the needle, may not clear clotted blood effectively.
Question
A 23-year-old man is brought to the ED in cardiac arrest secondary to trauma from a stab wound in the left side of the chest. Emergency 2D-echocardiography shows significant cardiac tamponade, likely due to leakage of blood from the heart. What is the best definitive treatment for this patient?
a. Defibrillate
b. Pericardiocentesis
c. Emergency department thoracotomy
d. High-quality CPR
Answer
a. Defibrillate
Rationale
A. Rationale: Sodium bicarbonate is the pharmacologic treatment of choice for pre-existing metabolic acidosis.
Question
A 24-year-old man is brought to the emergency department with fever, dehydration, and abdominal cramps due to persistent diarrhea. He is hyperventilating, and his arterial blood gases reveal metabolic acidosis. While attempting to rehydrate the patient, he goes into cardiac arrest. Aside from performing ACLS, what other treatment options should you consider to increase the chances of achieving return of spontaneous circulation?
a. Sodium bicarbonate
b. Magnesium sulfate
c. Naloxone
d. Amiodarone
Answer
a. Sodium bicarbonate
Rationale
A. Rationale: The patient is in pulseless electrical activity, and the primary causes are hypoxemia and hypovolemia. Blunt trauma to the chest may cause a lung injury, such as a tension pneumothorax. Cardiac tamponade and internal hemorrhaging can cause hypovolemia.
Question
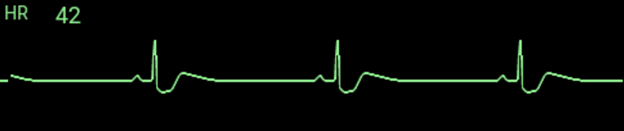
A 26-year-old man was kicked in the chest by a horse while attempting to removing its horseshoe. He was brought to the emergency department unresponsive and pulseless with occasional gasps. You record the following ECG:
Which of the following is NOT a likely reversible cause in this patient?
a. Pulmonary thromboembolism
b. Hypovolemia
c. Cardiac tamponade
d. Tension pneumothorax
Answer
a. Pulmonary thromboembolism
Rationale
A. Rationale: Hypothermia is a reversible cause of pulseless electrical activity. A body temperature of 34°C requires invasive rewarming techniques such as cardiopulmonary bypass while performing high-quality CPR. Another example of invasive rewarming is extracorporeal circulation. It is recommended that first responders bring a patient like this to a hospital equipped with such invasive treatments.
Question
A 27-year-old woman had been stranded inside her car during a blizzard. She went into cardiac arrest while being transported to the emergency department. Her vital signs on arrival are as follows: HR = 0 bpm, BP = 0 mm Hg, RR = 0/min, T = 34.0°C. ECG tracing is as follows:
Aside from CPR, what other intervention is necessary to increase this patient’s chances of achieving return of spontaneous circulation with no neurologic deficits?
a. Cardiopulmonary bypass
b. Passive rewarming
c. Epinephrine bolus injection
d. Rapid defibrillation
Answer
a. Cardiopulmonary bypass
Rationale
D. Rationale: After being shot, the patient is likely to have lost a significant amount of blood. The clinical signs and symptoms point to hypovolemic shock. A rapid infusion of crystalloid solution is the treatment for hypovolemia.
Question
A 28-year-old man is transported to the emergency department after being shot. He sustained gunshot wounds on the upper thigh. He is hypotensive, with a rapid heart rate, and appears diaphoretic and pale. Aside from the pain, he is feeling faint. What is the treatment recommended treatment for this patient?
a. Give rescue breaths
b. Initiate chest compressions
c. Give epinephrine
d. Rapid infusion of a crystalloid solution
Answer
d. Rapid infusion of a crystalloid solution
Rationale
B. Rationale: The patient has a tension pneumothorax likely iatrogenic from mechanical ventilation. On chest X-ray, the mediastinal structures and the endotracheal tube have shifted to the left. He is hemodynamically unstable because the cardiovascular structures are compressed. Definitive treatment is a chest tube thoracostomy wherein a chest tube is inserted in the right thoracic area to decompress the accumulated air and allow the lung to heal itself. Needle thoracostomy is not a definitive management. The small needle bore may be unable to decompress this large volume of air. It also carries a risk of being dislodged and producing another pneumothorax.
Question
A 45-year-old man has been in the ICU for 7 days now post cardiac arrest secondary to an MI. His oxygen saturation has not been above 94%, even while on mechanical ventilation. A stat portable X-ray shows the following:
https://radiopaedia.org/articles/tension-pneumothorax
Vital signs are the following: HR = 49 bpm, BP = 70/40 mm Hg, T = 36.8°C. What is the definitive treatment for this patient’s condition?
a. Extubate the patient
b. Chest tube thoracostomy
c. Needle thoracostomy
d. Norepinephrine infusion
Answer
b. Chest tube thoracostomy
Rationale
B. Rationale: The attending healthcare provider must know when to defer CPR. CPR is futile in this case as the patient already exhibits rigor mortis.
Question
A 45-year-old man was brought into the emergency department by his relatives. They reported that he allegedly hanged himself in his room and do not know when the incident happened. While assessing the patient, you notice that his joints and muscles are already stiff. He is hooked to a cardiac monitor, and the following ECG tracing is recorded:

What is your next course of action?
a. Call for help and activate the emergency response team
b. Defer resuscitative efforts as CPR is futile in this case
c. Begin high-quality CPR with two ventilations every 30 chest compressions
d. Defibrillate the patient
Answer
b. Defer resuscitative efforts as CPR is futile in this case